Rapidly evolving scope of practice means that traditional community pharmacy workflows need review. What works (and what doesn’t)?
The range of professional services delivered by community pharmacists has expanded rapidly in recent years, from vaccination to UTI prescribing and beyond. As
these services increase in popularity, they are shifting from ancillary service to core business.
This widening scope is forcing community pharmacies to review how they conduct their business and the way front-of-house staff interact with patients.
No longer is dispensing prescriptions on a first come, first served basis sustainable. With adjustments to workflow, vaccinations and other booked services have been prioritised and run simultaneously, says Queensland-based prescribing pharmacist Kate Gunthorpe MPS.
‘We are moving away from the mindset that dispensing always comes first. We need to triage effectively and manage expectations, so every patient feels seen and cared for,’ she says.
And it isn’t just about sequential processes. Workflow changes also require a shift of communication approaches and pre-existing mindsets around professional service provision.
‘The biggest pitfall I’ve discovered is apologising for charging or determining that the consultation wasn’t worth charging for,’ Ms Gunthorpe says. ‘That instantly undermines the service’s value. Every consultation, whether the outcome is a prescription, advice or reassurance, involves clinical reasoning, professional judgement and patient care.’
So, how should the profession move forward? The PSA’s foundation documents are clear that all services must remain patient-centric.
That means redesigning workflows on the floor, developing new communication strategies for staff and providing additional training for pharmacy assistants to ensure a consistent, professional patient experience.
AP spoke with Ms Gunthorpe and pharmacy assistant Madison Low about adapting workflow to integrate services without disrupting dispensing. product or medicines transaction. I now explain that I will assess their presentation, then create a unique shared management plan for them – which may or may not involve a prescription. Setting that expectation upfront helps enormously.
Case 1 Kate Gunthorpe MPS
Pharmacist prescriber, Implementation and Change Specialist, TerryWhite Chemmart, Samford, Queensland

Our team started by mapping our busiest times to understand where bottlenecks occurred. We then built clear workflows – for example, using a booking system for consultations where possible, and ensuring at least one pharmacist remained consult-focused during every day.
We trained our assistants to triage appropriately and use consistent language, such as ‘the pharmacist will see you shortly for your consultation’, which helped the process feel deliberate rather than disruptive. Once the team understood that consultations were core services, not interruptions, the process flowed more smoothly.
Patients often expect a prescription outcome from a consultation, so I changed the framework, ensuring the consultation became a clinical one, not a product or medicines transaction. I now explain that I will assess their presentation, then create a unique shared management plan for them – which may or may not involve a prescription. Setting that expectation upfront helps enormously.
When we changed our front-of-shop language, patients stopped viewing consultations as waiting in a queue. That one shift in language lifted the professionalism of the whole process; patients were more patient, staff felt more confident explaining the service, and we saw an improvement in how people valued the pharmacist’s time.
One thing I would advise other pharmacists about charging appropriately for their time, even when the consultation doesn’t end with a script, is to start valuing their expertise. The consultation is the service, not the outcome. We’re expertly trained to assess, diagnose and provide evidence-based care. That deserves to be remunerated. Once pharmacists stop apologising and start consistently charging for their time and expertise, patients begin to respect that boundary too.
I find it is better to be transparent and consistent with pricing. I explain what’s included in the consultation, so patients understand what they’re paying for. Most importantly, I believe in it myself. If you hesitate to charge, your team and patients will pick up on that.
The work floor also needs redesigning to normalise consulting services as part of everyday care. It starts with the physical layout and staffing models. Pharmacies should expect consultations to happen and allocate dedicated private spaces, clear booking systems and enough pharmacist coverage, so that one can focus on clinical care, while others oversee dispensing and other services. Culturally, it’s all been about mindset: we stopped treating services as extra and started treating them as central to what we do.
That meant redistributing roles, upskilling support staff with more autonomy to triage and manage appointments, and introducing appointment blocks.
The effect of all these new processes has resulted in major change. Our pharmacy assistants are our front line, and their language is setting the tone for the entire patient experience. We have invested time in scripting and role-playing, so that the assistants feel comfortable discussing new services. The staff have learned to understand what each service involves, how long it typically takes, and when to book or triage patients.
Scripts no longer automatically take priority over walk-up service requests. They are both core services. Pharmacies are healthcare hubs where patients can expect to have a prescription filled but also be able to discuss their health concerns.
Patients also value honesty and clarity. If a medication is not appropriate, explaining why builds understanding and trust – especially when you provide alternative options or safety net advice.
Because pharmacy staff use consistent, confident language and understand the workflow, everything runs much more smoothly. It has also empowered the staff to take pride in being responsible for a part of the patient care process, not just the retail side.
When staff describe services as core health care, not as ‘extras’ or ‘add-ons’, patients have started to see the pharmacist as a clinician involved in their primary care.
It’s a subtle but powerful mindset shift that’s transforming how the pharmacy is perceived.
Case 2 Madison Low
Retail manager, TerryWhite Chemmart, Arana Hills, Queensland

Since we started offering services like UTI consultations and vaccinations, my role has expanded significantly. We no longer just provide products; we’re delivering a more complete healthcare solution.
A person recently came to the counter, visibly frustrated because they had symptoms of a urinary tract infection but couldn’t get in to see their doctor. They were holding a box of Ural.
Rather than just selling them the product, I suggested they talk to the pharmacist, assuring them that in many cases the pharmacist can provide a full treatment without needing a doctor’s visit.
I asked a few questions about their symptoms, then checked with the pharmacist to confirm a consultation was possible immediately. It was, and not long afterwards the patient went away happy.
Asthma management is one of the most common chronic conditions we see. Many patients believe they understand how to manage the condition, especially because they can access inhalers over the counter. But often that’s not the case. One of my roles is to let patients know there may be better solutions. Our pharmacists can review their current treatment and provide an improved management plan.
Since becoming more mindful of the language I use with patients, I’ve noticed a positive change in how they respond to me.
By communicating in a more empathetic and approachable way, I’ve found patients are more comfortable asking questions and discussing their concerns. This has made it easier to identify when a patient might benefit from a review with one of our pharmacists.
This change in language has also strengthened trust between patients and the pharmacy team. Patients seem more engaged and confident in the care they receive, and I feel more confident in my role as a link between them and our pharmacists.
The biggest challenge has been balancing our time – especially during busy periods like the flu season, when there are lots of vaccines to administer, prescriptions to dispense and consultations to organise. I’m proud of how our team works together to ensure our patients are looked after promptly and get the attention they need.



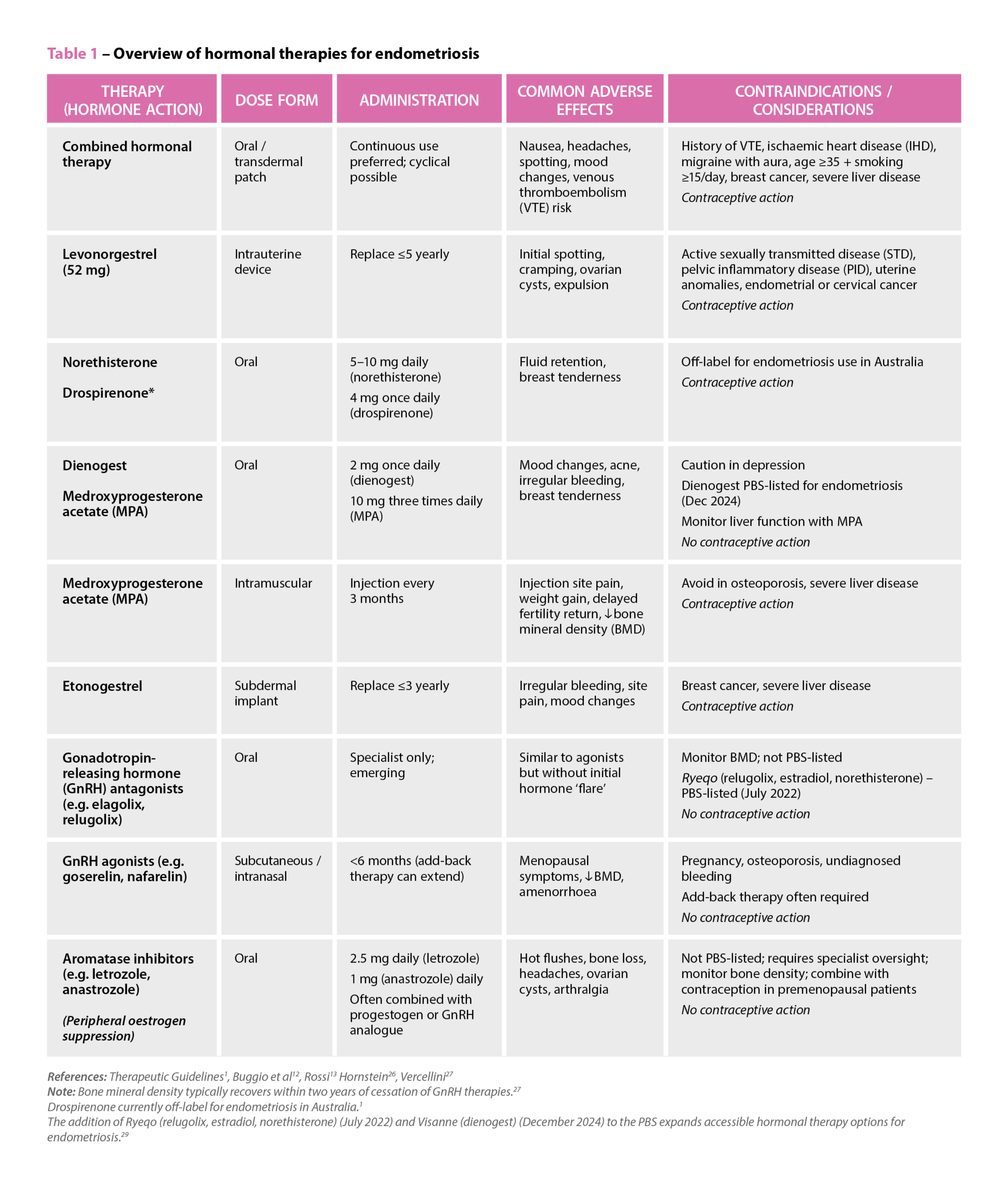 References: Therapeutic Guidelines
References: Therapeutic Guidelines

 Genevieve Adamo MPS (Image: Steve Christo Photography)[/caption]
Genevieve Adamo MPS (Image: Steve Christo Photography)[/caption]







