
As a pharmacist who cares about people, any extra involvement of having pharmacists in aged care is going to be good. It’s going to be the best thing for the residents and the nursing staff and everyone to have us there – extra information about medicines, extra safety checks on medicines, and just that constant presence that pharmacists are trained so well to have. So, in essence, it’s fantastic.
But putting on my work hat, we can’t help but wonder how it’s going to work. Because we have trouble finding pharmacists right now for the current model. So I don’t know how they’re going to find a pharmacist for each aged care facility, even if it’s only one day a week. Those pharmacists just don’t exist.
We have about 220 facilities across the country and it’s a constant challenge keeping up the workforce.
Secondly, you can’t help but wonder what’s going to happen to the current funding model. So surely if they’re dishing out $350-odd million, they’ll have to replace the current $20 million or so that is spent on RMMRs and follow ups and QUMs in aged care right now. So we are desperate to know the details of how the funding will be rolled out.
Aged care is not a very sexy place to work and it’s had some very bad press. So there’s not many people that want to work in aged care generally. Combine that with a general shortage of pharmacists everywhere, and you get not many people willing to do what we do.
Medication review is a very important function. But as the Quality and Safety Commission increases the reporting that’s required of nursing staff around medication use, psychotropics, polypharmacy, and now opioids and the ongoing concern with antimicrobial use, pharmacists are best placed to be able to comment on the use of all those medications.
Just having someone looking at a spreadsheet who is not trained in medications, and saying, ‘Oh, that person shouldn’t be on that anymore’, is not best medicine.
Pharmacists can look at the information, but then also, pharmacists are so well trained to deal with everyone across the whole spectrum for the residents. So we can talk to the GP in their language about the medicine, but equally we can talk to the family and the next of kin and the other people that make decisions for the residents about those medicines. They’re very different types of conversations. So you have to be quite well trained to be able to do that. And pharmacists have that.
We constantly get asked questions about medication storage, about S8s, S4Ds and S4Rs and how are they meant to be stored? What are the regulations? You really need a specialist in all that legislation. And the poor nursing staff just can’t keep up.
The one thing I try and find in our pharmacists is people who, at the heart of it all, they want to help. Because this is not a very sexy industry, it’s not very popular. So you really have to have that passion to help people using your knowledge.
So you have to be soft in the middle but you also have to be a bit hard on the exterior. You have to have quite a thick skin and be able to have extra communication skills to try and cut through and get the information you need, in our case for medication reviews, but also be able to educate nurses about medication. It’s quite a communication skill base that you’re after as well.
I did grow up in pharmacy. I had been hanging around pharmacy since I was born. My parents were community pharmacists. But they didn’t have an aged care facility. I just sort of fell into this because I have three children and I thought I could fit in the visits in school hours. That was about five years ago and since then I’ve worked out that it’s a lot more. I really am a firm believer that we can really help here. It really uses all your skills to actually help people.
The best examples are where I have really great invested GPs, and they like us to all sit together as a team to talk through the RMMRS. So recently, at one of my nursing homes I did a case conference with the GP and the nurse practitioner and the clinical manager from the facility. They all get paid to be there, I didn’t, but that’s okay. This was a resident who was cognitively impaired, but I could communicate with her about her medication. However, it was most important to be communicating with her daughter about medication because her daughter is making a lot of decisions.
We were able to try and get to the bottom of why she was on a lot of medications for her heart. There were a few prescribing cascades that had happened, no one really knew why she ended up on some of the medications and so we were able to come up with a plan together just to cut back some of those unnecessary medications and review some of her antipsychotics, so she felt better about her medicine. Her next of kin had a lot more information and the GP and the nurse practitioner had a plan to follow to try and improve her medication regimen.
She had been being hospitalised a lot. She’d had a lot of falls and things recently but I understand that decreased significantly. So if you can keep them from falling, keep them out of hospital, you will really improve their quality of life.
I think the challenge now for the industry will be providing all these embedded pharmacists. We need to think about how we’re going to get that flow through of people with those skills. We need to think about how we get them skilled up quite quickly. There aren’t enough pharmacists, so we need to think about what sort of levels of skills we can impart in people quickly, so that we can provide this service. And we need the government to tell us how they’re going to fund it soon so we can all get organised.




 ‘We’re increasingly seeing incidents where alert fatigue has been identified as a contributing factor. It’s not that there wasn’t an alert in place, but that it was lost among the other alerts the clinician saw,’ Prof Baysari says.
‘We’re increasingly seeing incidents where alert fatigue has been identified as a contributing factor. It’s not that there wasn’t an alert in place, but that it was lost among the other alerts the clinician saw,’ Prof Baysari says.

 Beyond the arrhythmia, AF often signals broader pathological processes that impair cardiac function and reduce quality of life and life expectancy.5 Many of these conditions are closely linked to social determinants of health, disproportionately affecting populations with socioeconomic disadvantage. Effective AF management requires addressing both the arrhythmia and its underlying contributors.4
Beyond the arrhythmia, AF often signals broader pathological processes that impair cardiac function and reduce quality of life and life expectancy.5 Many of these conditions are closely linked to social determinants of health, disproportionately affecting populations with socioeconomic disadvantage. Effective AF management requires addressing both the arrhythmia and its underlying contributors.4  C – Comorbidity and risk factor management
C – Comorbidity and risk factor management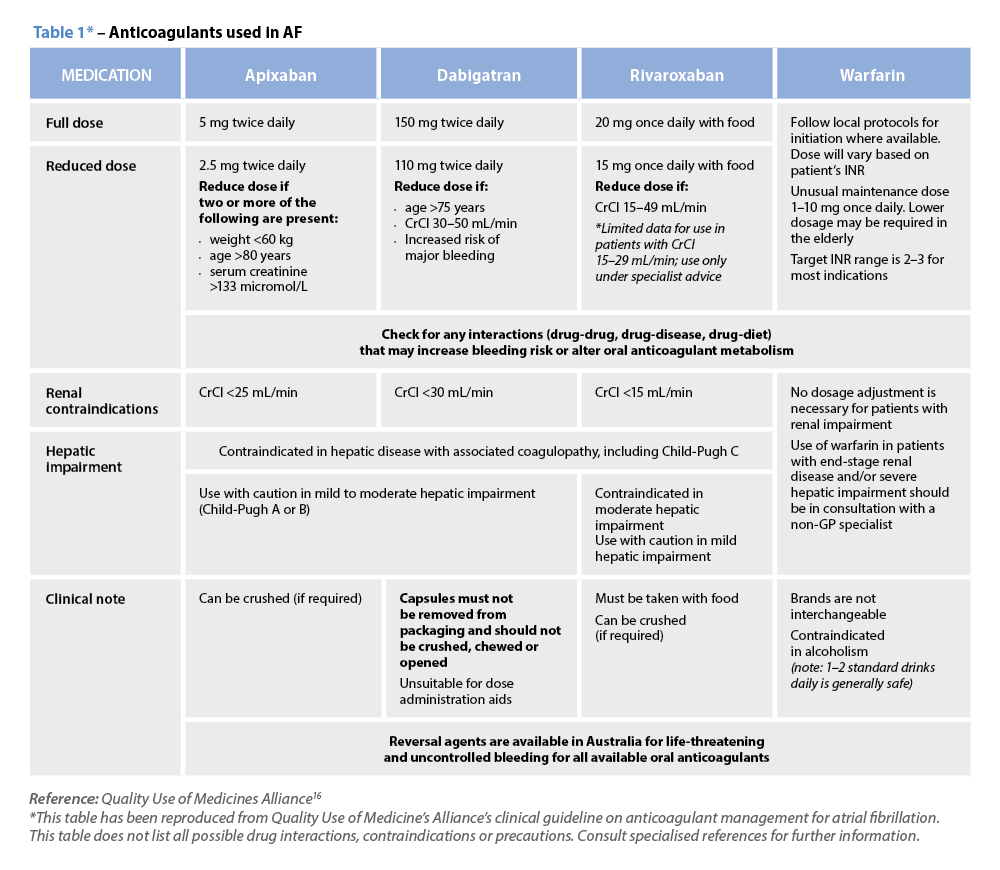 Warfarin
Warfarin



