The theme for this year’s World COPD Day (15 November 2023) is ‘Breathing is Life – Act Earlier’. Prevention, early diagnosis and optimal treatment are essential to reduce the progression of this irreversible disease.
In 2022, COPD accounted for over half (51%) of the disease burden due to respiratory conditions and 3.7% of the total disease burden in Australia.
Aboriginal and Torres Strait Islander peoples are 2.3 times as likely to have the condition than the rest of the population, with prevalence also spiking in those from lower socioeconomic groups.
Smoking is the number one risk factor for developing COPD, said Debbie Rigby FPS, Advanced Practice Pharmacist and Lung Foundation Australia COPD Clinical Advisory Committee member.
‘However, 30% of people with COPD have never smoked,’ she said.
 Reducing the burden of disease requires a wider focus targeting at-risk individuals early, who could have unidentified ‘pre-COPD’.
Reducing the burden of disease requires a wider focus targeting at-risk individuals early, who could have unidentified ‘pre-COPD’.
Construction workers at risk from silica and other workplace exposures
The hazards of workplace silica exposure in engineered stone used in domestic and commercial construction are a hot topic, with Bunnings recently announcing it will stop selling engineered stone by the end of 2023, Ikea’s decision to phase it out in Australian stores, and governments considering banning the materials.
In addition to causing silicosis, silica exposure can also cause COPD. But it’s not just engineered stone in kitchen benchtops which expose people to silica at work.
Silica exposure is a risk factor in other construction and industrial jobs, such as:
- tunnelling
- brick manufacturing
- pottery
- ceramics
- gold mining
- iron and steel founding
- other cement industry positions.

Along with these occupational hazards, genetic factors and early life events also play a role, including:
- air pollution exposure
- alpha-1 antitrypsin deficiency
- maternal factors leading to preterm birth or low birth weight
- exposure to passive smoking in early years of life
- early childhood infections.
While patients won’t be aware that they have reduced lung function, damage can be reversed when detected early on.
‘People typically don’t become symptomatic with COPD until they’ve lost around 30–50% of their lung function,’ said Ms Rigby. ‘That’s why identification in the early stages is so important.’
So how do you find the people who have never smoked, have no symptoms, but may have workplace exposure which places them at risk?
Early diagnosis
Previous case finding trials in community pharmacy have proven effective in identifying people who need to see the GP for spirometry to diagnose COPD.
Pharmacists can use the Lung Foundation’s lung Health checklist with Piko-6 screening to pick up at-risk patients.
‘The Piko-6 measures forced expiratory volume in 1 second over forced expiratory volume in 6 seconds,’ said Ms Rigby. ‘That ratio gives a traffic light indication of whether the patient is at risk for COPD.’
Pharmacists also need to help patients self-identify at-risk jobs which expose them to dust and other pollutants.
An optimised treatment approach
Early diagnosis with COPD is crucial to slow the progressive decline in patients’ lung function through appropriate therapy.
‘Most people with COPD will need long-acting bronchodilators – either alone or in combination,’ said Ms Rigby. ‘This will help to reduce symptoms such as shortness of breath, sputum volume and purulence, and cough.’
This treatment approach is twofold, helping to reduce the risk of future exacerbations. ‘Every time a patient with COPD has an exacerbation, their lung function declines and it doesn’t come back to where it was,’ she said.
Deb Hawthorne MPS, credentialed and GP pharmacist, often encounters patients who overuse inhaled corticosteroids, rather than first-line therapies such as long-acting β2 agonists (LABAs) or combination LABA and long-acting antimuscarinic antagonists (LAMAs).
‘I’ll say, “did you realise this isn’t the first-line indicated therapy, and there are risks associated with ongoing use?”’ she said.
Ms Hawthorne also directs patients towards the Lung Foundation’s COPD X stepwise approach, followed by a therapy recommendation to the GP.

Some people with COPD also have asthma, which is a degree of reversibility of the airway disease, said Ms Rigby.
‘These patients are likely to benefit from appropriate as-needed use of Short-Acting Beta Agonists (SABAs) to control any symptoms,’ she said.
People who just have COPD are still likely to benefit from SABAs, especially during an acute exacerbation.
‘However, pharmacists need to be vigilant about overreliance and overuse of SABAs in people with COPD,’ she said. ‘We need to always encourage them to use their long-acting bronchodilators, either alone or in combination.’
Correcting inhaler technique
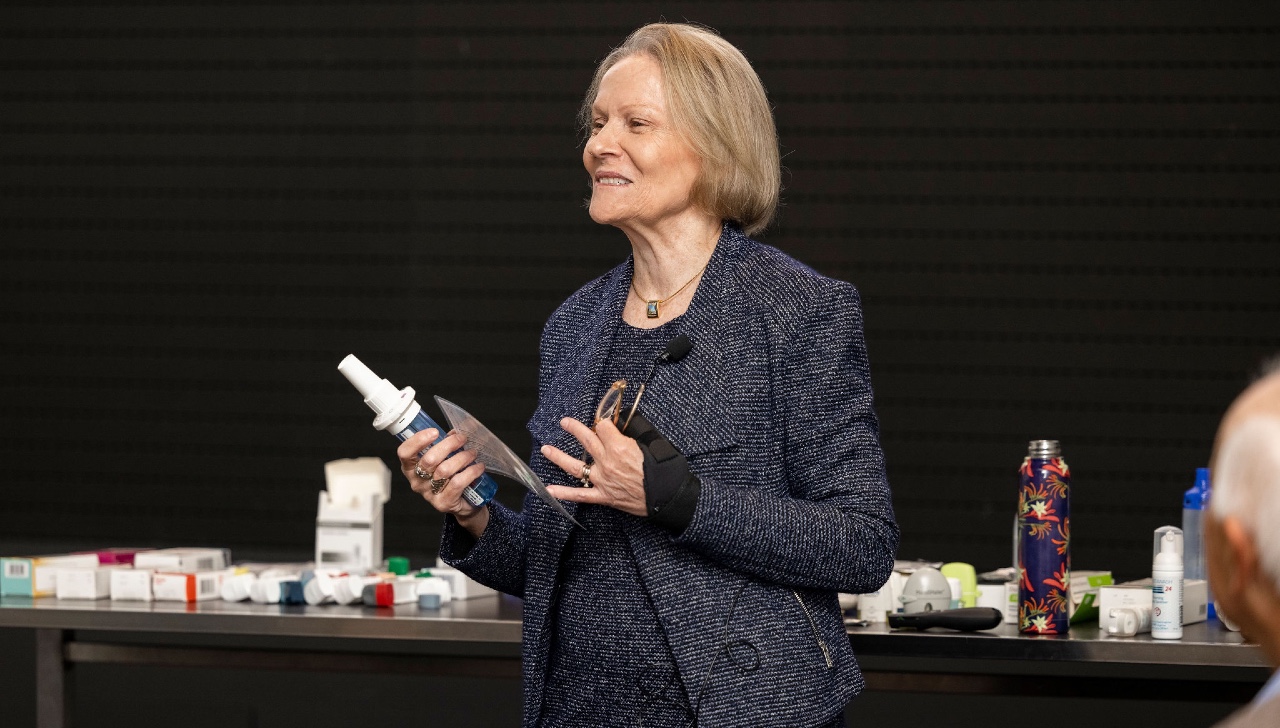
Up to 94% of people with COPD don’t use their inhalers correctly. ‘Community pharmacists should therefore be assessing patients’ inhaler technique at every opportunity,’ said Ms Rigby.
Ms Hawthorne places a concerted focus on inhaler technique in HMRs or patient consultations – which helps to identify any potential dexterity issues.
‘I’ll bring along a box of all the different placebo inhalers on the market to play with,’ she said. ‘We hold them, get a good grip, and see which one fits.’
HMR follow-ups provide an opportunity to assess whether adherence has improved. ‘One of my number one reasons for follow-ups is to assess inhaler adherence,’ said Ms Hawthorne. ‘It’s brilliant to see people improve.’
Increasing lung health
Aside from smoking cessation, pulmonary rehabilitation is also ‘incredibly beneficial’ for people with COPD by providing exercises and self-management strategies to cope with everyday activities and exacerbations, said Ms Rigby.
This includes two-four breathing exercises, which entails breathing in over 2 seconds, then breathing out in a slow exhalation over 4 seconds while looking at a rectangle shape.
‘Even things like holding a handheld fan over the lower part of the face can help both psychologically and physiologically reduce breathlessness,’ she said.
In Ms Hawthorne’s experience, patients often attend pulmonary rehab after a hospital visit for a COPD exacerbation. But she suggests patients keep at it.
‘Every time patients go to pulmonary rehab, they pick up a different piece of education or advice,’ she said. ‘So, I encourage patients to do it multiple times.’
1,000 mg lifetime prednisone dramatically increases risk of other comorbidities
Comorbidities such as cardiovascular disease (CVD), osteoporosis, reflux and anxiety and depression increase the risk of COPD exacerbations, said Ms Rigby.
‘As little as 1,000 mg cumulative lifetime dose of prednisone to treat acute COPD exacerbations very much increases the risk of developing osteoporosis, type two diabetes, cataracts and glaucoma,’ she said.
For someone taking a 50 mg prednisone dose, that’s only 20 doses.
Pharmacists can check patients’ dispensing history to identify how many prescriptions of prednisone they have had over time along with:
- referring them to a GP for assessment
- suggesting light weight-bearing exercise
- recommending calcium and vitamin D supplements.
A leading cause of death in patients with COPD is CVD. So during HMRs, Ms Rigby screens patients with COPD using a cardiovascular risk calculator.
Symptoms of heart failure can mirror those of COPD, including shortness of breath – making it challenging to identify the root cause.
‘But optimising treatment for both COPD and heart failure can reduce a patient’s symptoms and their risk of exacerbations,’ said Ms Rigby.
Learn more about COPD and respiratory care from Debbie Rigby herself at PSA’s Credentialed Pharmacists Conference, CPC24, in Cairns from 3-5 May 2024. Registrations are open now.



 Kelly Abbott MPS[/caption]
Kelly Abbott MPS[/caption]


 Owner of Canberra's Capital Chemist Southlands Louise McLean MPS.[/caption]
Owner of Canberra's Capital Chemist Southlands Louise McLean MPS.[/caption]

 Supplied by CSL Seqirus[/caption]
Supplied by CSL Seqirus[/caption]