It is difficult to overstate the importance of the present and potential future role of the pharmacist in the day-to-day health care of most Australians.
Surveys of consumer patterns in utilising the health system, including those conducted by the Consumers Health Forum (CHF), find, typically, that there is no other health professional with whom a consumer interacts more than their local pharmacist.
Perhaps because of this familiarity, many consumers take their local pharmacist and the role they play for granted. However, there is also a tension between the clinical and retail activities of pharmacy: there is a view among consumers that community pharmacies don’t necessarily feel like health settings given their strong retail focus. So, it is the mix of the ubiquity of pharmacies, their retail/health setting and potential to serve as a health destination which helps explain the keen interest of the CHF in advancing the pharmacists’ role in our health care.
The CHF has been a strong advocate of a more active role for pharmacists in primary healthcare in ensuring best possible care, particularly for those with chronic illness. Much of modern health care can be delivered more effectively when it is provided and coordinated in the community, at or near the patient’s home.
We are in an age where consumers demand a responsive healthcare system, are vocal about the characteristics of the system they want protected and have expectations about the directions future healthcare should take. Pharmacists should make routine the quality use of medicines including support for patients to take the right medicines at the right time. It should safeguard against medication mistakes which are too frequent and cause great cost in terms of patient suffering and in overall health expenditure.
There is also the expanding array of routine services that can fall within the pharmacist’s realm whether it be immunisation, blood pressure checks or other services. We have supported the PSA in its work to develop and promote the role of pharmacists in primary health care within the scope of their training and expertise. The Pharmacists in 20231 report is a comprehensive vision for the direction Australia’s pharmacists and the healthcare community need to take to meet consumer needs in the 21st century.
Person-centred care
Pivotal to this direction for the future is consumer-driven person-centred care, with pharmacists playing a broader role. That was a key finding that emerged from a forum and a population survey CHF was commissioned to conduct by PSA in 2017. The survey and forum found that consumers recognise the wider range of roles pharmacists can and should play. Consumers value pharmacists’ expertise on medication provision and feel that greater use of and access to this expertise would be appropriate and useful.
Consumers see pharmacists as offering access to care in a way that other health professionals cannot. They are easier to access given that other practitioners largely rely on appointment-based services. Though there were stigma concerns raised by consumers with HIV and users of needle and syringe programs at pharmacies, consumers were confident that better training for pharmacists could overcome these attitudes.
In fact, it does appear education of consumers about the skills that pharmacists can offer should broaden the common consumer view of pharmacists’ services being limited to medicines advice and wound management.
Key conclusions from the CHF project included that PSA should work with pharmacists to improve standards of core professional services and that a register of specialist pharmacists be developed for consumers with specific health conditions. However, it remains unclear about how willing consumers would be to pay for a greater range and accessibility of services.
Value-based care
For consumers, the definition of value-based care incorporates more than just the cost of treatment, but also quality and experience of care. A pressing area for greater involvement of pharmacists is in services for Indigenous Australians for whom pharmacy services are often meagre, despite their much higher prevalence of ill-health.
The project involving PSA, the National Aboriginal Community Controlled Health Organisation (NACCHO) and James Cook University to embed pharmacists in 22 Aboriginal community-controlled health services in Queensland, Victoria and the Northern Territory is a welcome step.
A thread running through consumer involvement is the role of health literacy and patient activation. CHF envisages that pharmacy practice has a key role in supporting those struggling with health information as well as gauging how inclined patients are to adhere to a care plan and what can be complex medications regimes.
A recent Australian Bureau of Statistics survey2 found that in general, people with chronic illness or those experiencing psychological distress are less likely to feel positive about their health literacy. Literacy could be shared during a range of common pharmacy opportunities including help with understanding a vaccination chart, reading a prescription and explaining medicine side effects. The literacy role will become more significant as additional pharmacy services are developed.
Barriers to healthcare setting
There is a sense among consumers that community pharmacies do not feel like health settings. The aspirations for pharmacy to become much more integrated into the clinical care world still faces significant barriers.
Consumers would like to see greater availability of pharmacists to engage with consumers, and the provision of facilities in pharmacies that enabled confidential health discussions. What is emerging, however, is that pharmacists are doing more outside the traditional dispensing activity than ever.
A University of Canberra study3 of last year, identified five areas of community pharmacy interventions: clinical interventions, medication reviews, health promotion, screening and management of chronic diseases, and support services for drug addiction. These interventions had led to improved asthma control, detection of diabetes and cardiovascular risk factors, reduction in smoking rates and weight, and identification of drug-related problems.
The availability of vaccination services in pharmacies has contributed to increased vaccination rates. Through support programmes for drug users, transmission rates of blood-borne diseases decreased. Community pharmacies were well located to deliver comprehensive healthcare services due to convenience and accessibility. Despite this, the clinical interventions provided in pharmacies appeared not to be coordinated.
The study concluded that there is sufficient evidence for the effectiveness of most of the pharmacy services reviewed. However, the potential of the individual services might be further enhanced by interlinking the services and better integrating them with the patient care provided by GPs and other health professionals.
Integrated services
Quality care from the standpoint of a consumer, particularly those with one or more chronic conditions, is continuous, comprehensive and coordinated. This consumer expectation and the dynamics and technology of modern health care are driving pharmacy towards more integrated services in a variety of ways. A real question – and opportunity – to be explored in the current policy environment is what role can pharmacists play in emergent models of care such as patient and family centred health care homes?
Technology, whether it be eHealth developments like My Health Record, or the growth in point-of-care testing, is expanding the potential involvement of pharmacists in day-to-day medicine decision-making and management.
In aged care, one of the significant triggers for the current Aged Care Royal Commission has been allegations of poor medication practice and a litany of adverse events, underlining the need for more active oversight by pharmacists. The medical profession questions the widening scope for pharmacists, suggesting it weakens the rigour and responsibility of the practice of medicine. There is a strong measure of self-interest from both doctors and pharmacists in what could be portrayed as merely a demarcation conflict.
Expanded role for pharmacists
Of fundamental importance, however, should be what is in the best interests of the patient. CHF advocates an expanded role for pharmacists to promote quality and safety in access to medication. The Grattan Institute has put a persuasive case.4
As that report says, pharmacists are highly trained, have deep expertise in medicines, are among the most trusted of all professionals, and are located in most communities. Yet their role is far more limited than in many countries.
‘Broadening the role of pharmacists should not undermine GPs. The work of the pharmacist in primary care should only be in collaboration with the GP. For this reason, pharmacist prescribing in the community should be within the context of a structured prescribing arrangement with each GP,’ the Grattan report said.
There are compelling grounds for consumers and the professional pharmacy and medical bodies to join in scoping greater integration of care in areas such as those identified in the Grattan report including adverse drug interaction checks particularly with chronic-care patients, compliance packaging of medicines and advising GPs and other practitioners on patient care plans.
Medicines safety is an area of vital importance in developing pharmacists’ greater involvement. As the PSA report Medicine Safety: Take Care5 stated, 250,000 hospital admissions a year result from medicine-related problems. The report stated that three in five hospital discharge summaries where pharmacists are not involved in their preparation have at least one medication error. Possible options for better supporting medicine safety, such as dose administration aids, My Health Record and other digital health initiatives are measures that could support medicine safety.
Funding reform
So what are system-wide steps we need to stimulate the full benefit of the pharmacists’ expertise? It starts with funding reform. CHF believes Community Pharmacy Agreement (CPA) funding should be used more broadly across community pharmacy, not just in the narrow retail pharmacy setting. We put this view in our submission to the Review of Pharmacy Remuneration and Regulation.
Consumers say they want pharmacists working more closely with GPs as part of integrated primary care services. Measures to support this under future pharmacy agreement arrangements would be firmly in keeping with and help consolidate the Health Care Home model of care: a flagship area of primary care policy.
But the CPA arrangements are not a panacea. There should be a mix of funding arrangements that support the role of pharmacists in primary care teams, in supporting safe transitions out of hospital and in supporting quality use of medicines in high-risk settings like residential aged care. These include the Medicare Benefits Schedule and specific-purposes payments such as an expanded Workforce Incentive Program and PHN-funded and led innovations. Recent studies in Australia and abroad demonstrate consumer support for the principles of pharmacist integration into primary care and other settings.
No matter the setting, consumers want collaboration not competition between members of their care team, not measures that promote a fragmented system prone to further dysfunction, and for the quality and safety of the care they receive to be paramount. This is what true patient-centred care is about.
References
- Pharmacists in 2023: For patients, for our profession, for Australia’s health system. Canberra: The Pharmaceutical Society of Australia; 2019. Available from: psa.org.au/advocacy/working-for-our-profession/pharmacists-in-2023/
- Australian Bureau of Statistics. National Health Survey: Health Literacy. 2018. At: abs.gov.au/ausstats/abs@.nsf/mf/4364.0.55.014
- Buss VH, Shield A, Kosari S, et al. The impact of clinical services provided by community pharmacies on the Australian healthcare system: a review of the literature. Journal of Pharmacy Policy and Practice 2018. Epub 2018 August 27. At: https://joppp.biomedcentral.com/articles/10.1186/s40545-018-0149-7
- Duckett S. A mixed model is best for pharmacist prescribing. Grattan Institute submission to the Pharmacy Board of Australia discussion paper on pharmacist prescribing. March 2019. At: https://grattan.edu.au/submissions/a-mixed-model-is-best-for-pharmacist-prescribing/
- Medicine Safety: Take Care [Internet]. Canberra: The Pharmaceutical Society of Australia; 2019. Available from: https://www.psa.org.au/advocacy/working-for-our-profession/medicine-safety/ (edited)
- Wells L. The future of pharacy is in the primary care sector. Consumers Health Forum of Australia 2018. News & Media blog. Epub May 17, 2018. At: chf.org.au/blog/future-pharmacy-primary-care-sector




 ‘We’re increasingly seeing incidents where alert fatigue has been identified as a contributing factor. It’s not that there wasn’t an alert in place, but that it was lost among the other alerts the clinician saw,’ Prof Baysari says.
‘We’re increasingly seeing incidents where alert fatigue has been identified as a contributing factor. It’s not that there wasn’t an alert in place, but that it was lost among the other alerts the clinician saw,’ Prof Baysari says.

 Beyond the arrhythmia, AF often signals broader pathological processes that impair cardiac function and reduce quality of life and life expectancy.5 Many of these conditions are closely linked to social determinants of health, disproportionately affecting populations with socioeconomic disadvantage. Effective AF management requires addressing both the arrhythmia and its underlying contributors.4
Beyond the arrhythmia, AF often signals broader pathological processes that impair cardiac function and reduce quality of life and life expectancy.5 Many of these conditions are closely linked to social determinants of health, disproportionately affecting populations with socioeconomic disadvantage. Effective AF management requires addressing both the arrhythmia and its underlying contributors.4  C – Comorbidity and risk factor management
C – Comorbidity and risk factor management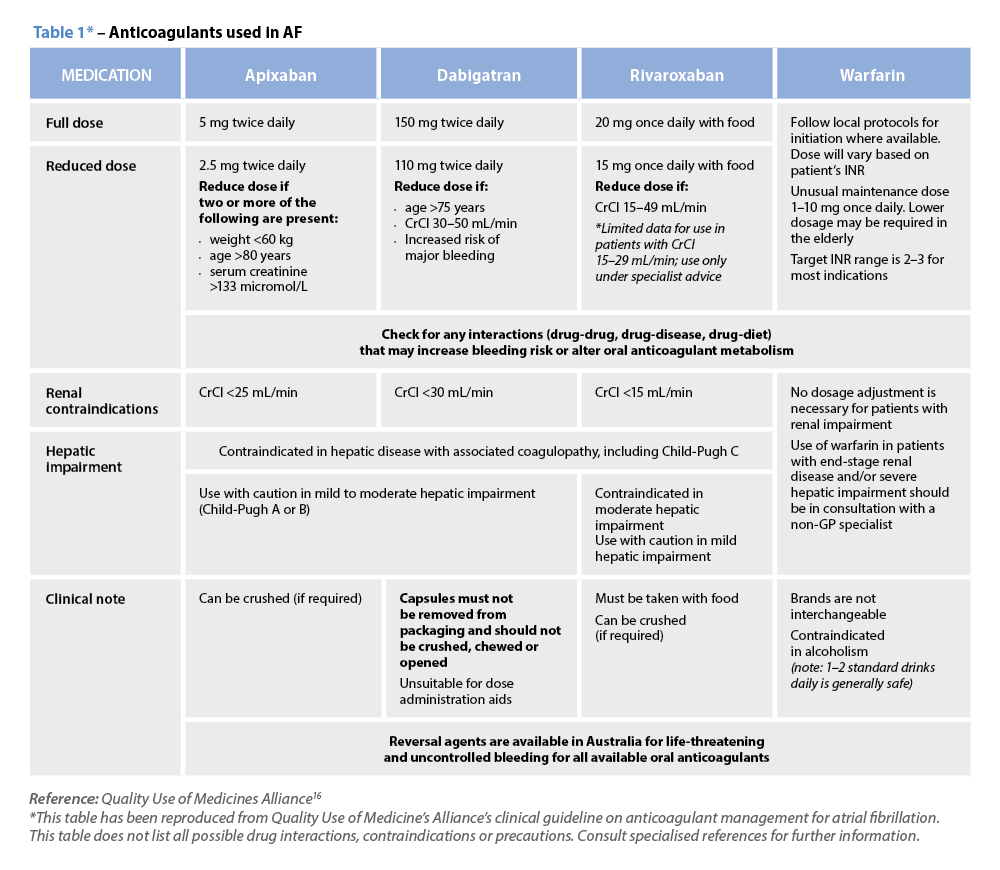 Warfarin
Warfarin




