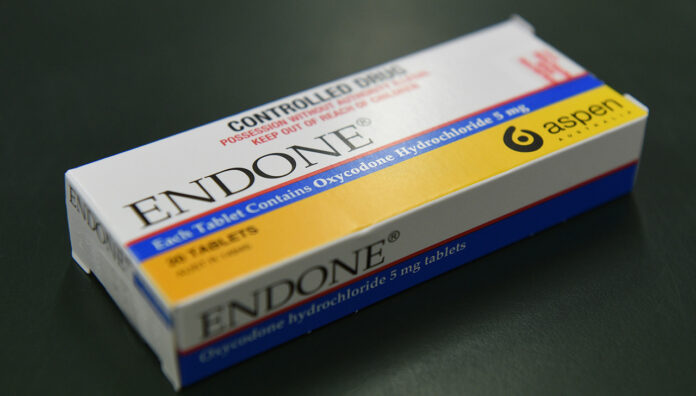
Oxycodone is the most prescribed strong opioid in Australia. Yet little was known about its use and prescribing patterns – until now.
Marketing and prescribing of oxycodone fuelled the opioid epidemic in the United States, still raging almost 30 years after the drug was first introduced.
To understand the previously unmapped associations between Australia’s oxycodone use and sociodemographic factors, UNSW researchers from the Medicines Intelligence Centre of Research Excellence and the National Drug and Alcohol Research Centre (NDARC) analysed linked data from 800,000 patients on PBS medicines dispensed, Medicare claims, hospitalisations and emergency department (ED) visits between 2014–2018.

While the research centres on oxycodone use in NSW, lead researcher Dr Malcolm Gillies said the findings are representative of the Australian population.
‘There’s not much difference between NSW and Victoria in prescribing, which accounts for most of the population.’
Older Australians are more likely to be new users of oxycodone
Initiation rates of oxycodone follow an age gradient, with the average age of new users being 54.7 years of age.
‘Among our oldest age category, which is 85 years and older, patients were started on opioids on average three times more often than those in the youngest age group (18–24),’ said Dr Gillies.
Higher prescribing rates of oxycodone in older patients relate to the higher disease burden in this demographic.
‘For example, there’s a higher prevalence of falls and cancer, which are precursors to opioid use,’ he said. ‘But the higher risk of adverse events with opioid use in older patients is something to bear in mind.’
Women are more likely to be initiated on oxycodone than men
An unexpected finding was the ‘definite blip’ of oxycodone use among women of childbearing age (18–44), who have ‘significantly higher’ initiation rates than their male counterparts.
Oxycodone is commonly used after hospital discharge in Australia. But because younger age groups use the opioid less frequently, there’s a distinct reason why prescribing rates are higher among females.
‘Looking at the list of diagnoses in the hospital episodes that precede the start of oxycodone, caesarean sections are quite high on the list.’
Regional and remote use is higher, but socioeconomic status doesn’t factor in
Echoing other research about patterns of opioid prescribing, oxycodone was initiated more frequently in areas outside major cities than in urban areas.
Injury rates are typically higher in rural areas as opposed to urban locations, which is a key differentiator in opioid prescribing, said Dr Gilles.
‘Those injuries tend to be more severe, with longer-term consequences,’ he said. ‘Specialist services are also harder to access outside cities, including chronic pain services – which are important down the line.’
However, there was one distinct variation. ‘Unlike other studies, we didn’t see that oxycodone use varied according to socioeconomic status, once we accounted for where people were living, their gender and age,’ he said.
A proportion of the population will become long-term oxycodone users
Patients were typically prescribed oxycodone post-hospital discharge, after a therapeutic procedure, or ED visit, together accounting for half of all initiations.
‘On the other hand, hospital admission for injury or a past-year history of cancer were less common reasons for oxycodone initiation than surgery,’ said Dr Gillies.
Most of the time (two thirds), patients were only dispensed a single pack of PBS oxycodone. But 4.6% of people had a recent dispensing of oxycodone a year after initiation.
‘Even after a serious operation we would expect the need for oxycodone to relieve pain would be over by 90 days,’ said Dr Gillies.
‘The fact that a proportion of people were taking oxycodone 12 months later underlines the need for early, careful assessment of ongoing pain to maximise appropriate use of non-opioid and non-pharmacological pain control.’
While there was no data available on the reason for dispensing at the 12-month mark, Dr Gillies said it was presumably due to an ongoing need for analgesia.
‘Among trauma patients, persistent use is much more common, which is well known in the literature,’ he said. ‘If you have a serious injury and difficult recovery, that might lead to some form of chronic pain.’
While the research didn’t delve into the appropriateness of use, oxycodone prescribing was more often than not for ‘plausible reasons’, including tonsillectomy, or hip and knee replacements. But this wasn’t always the case.
‘There was more room for variation in some cases, including presentations to ED for backache or acute abdominal pain,’ said Dr Gillies.
Recent research revealed that opioids don’t help acute non-specific lower back or neck pain. Other studies have found that physiotherapy is an effective non-pharmacological alternative for ED backache presentations.
‘That can sometimes mean patients don’t need to receive an opioid,’ he added.
The research doesn’t tell the full picture
One shortcoming of the research is that other prescribed opioids, available via private prescription, were not recorded. Codeine was also accessible over-the-counter during part of the study period, said Dr Gillies.
‘That means we couldn’t see if people were switching between oxycodone and codeine, for example,’ he said. ‘So we may have underestimated the long-term use.’
Better access to data, including GP data linked to the other data sources such as specialist prescribing, would provide a broader idea of oxycodone use, and improve development of healthcare policy and initiatives.
‘Australia has a fragmented healthcare landscape, so getting data about what happens in every corner is a bit of a jigsaw puzzle,’ he said.
Dr Gillies thinks the difference between city and rural oxycodone prescribing should also be further explored to ensure use is appropriate outside metropolitan areas.
‘We’ve got a follow-up study coming soon which specifically looks at use after hospital discharge’ he said. ‘So watch this space.’
Oxycodone use is trending downwards
While there was a slight increase in oxycodone prescribing from 2014–2017, use tapered off again from 2017–2018, said Dr Gillies.
‘That includes the level of people starting oxycodone for the first time, the level of people who were ongoing users and the proportion of oxycodone among all opioids.’
This downward trend suggests some of the policy levers which have already been pulled – including PBS-listing changes, prescribing restrictions, and real-time prescription monitoring – are working.
‘We don’t know whether they’re increasing appropriateness, but they are certainly decreasing use,’ he said.



 Kelly Abbott MPS[/caption]
Kelly Abbott MPS[/caption]


 Owner of Canberra's Capital Chemist Southlands Louise McLean MPS.[/caption]
Owner of Canberra's Capital Chemist Southlands Louise McLean MPS.[/caption]

 Supplied by CSL Seqirus[/caption]
Supplied by CSL Seqirus[/caption]