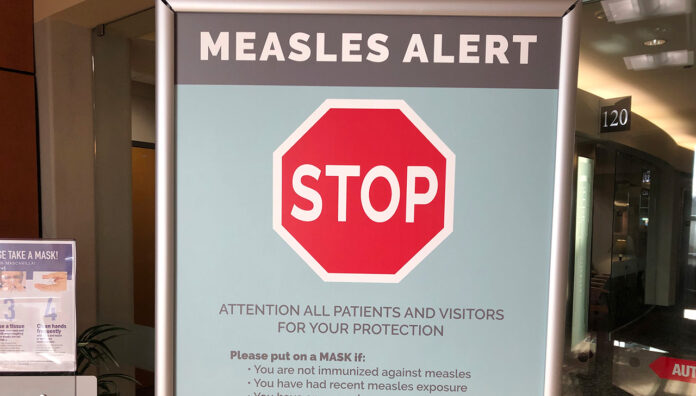
With measles cases climbing across Australia and pharmacies increasingly listed as exposure sites, community pharmacists must be prepared.
Earlier this year, a patient who had just returned from Vietnam walked into Advantage Chesterville Pharmacy in Melbourne with a script for antibiotics.
‘She was wearing a face mask, and when I spoke to her she just said that she had a cough but she wasn’t sure what the cough was from,’ said community pharmacist Minh Ngo MPS, who was on duty when the patient came through.
Some time later, the pharmacy received word that the patient was infected with measles.
‘She either informed the hospital or the GP, but we just got a call from the [Victorian] Department of Health to notify us that we were an exposure case,’ she said.
With measles spreading around Australia at an unprecedented rate, this is a position many pharmacists may soon find themselves in.
Victoria is in the midst of its worst measles outbreak in a decade, with 25 cases recorded so far this year. New South Wales and Western Australia are not far behind, with 21 and 18 cases reported respectively.
Healthcare settings such as pharmacies have been increasingly listed as exposure sites as people seek treatment for the highly infectious and virulent disease.
Australian Pharmacist explores the steps pharmacists should take when confronted with this predicament.
Patient contact tracing
When a healthcare setting such as a pharmacy becomes a measles exposure site, it is responsible for contact tracing.
‘We had to inform every patient who was in the [pharmacy] at that time that we were informed that the exposure might have happened,’ Ms Ngo said.
This includes asking patients if they have any symptoms. Early symptoms of measles, before the rash appears, include:
- fever
- tiredness
- cough
- runny nose
- sore red eyes
- malaise.
‘We had to inform every patient who was in the [pharmacy] at that time that we were informed that the exposure might have happened.’
MINH NGO MPS
Post-exposure testing and prophylaxis
All symptomatic patients who were exposed to measles need to follow specific protocols.
‘We told them that if they have any symptoms, if they develop any cough or if they have any concerns then go and get tested,’ Ms Ngo said.
Patients who have attended a known exposure site should be offered the Measles, Mumps, and Rubella vaccine within 72 hours of measles exposure to avert infection. In those who are unvaccinated or partially vaccinated, particularly young infants, pregnant people,, or immunocompromised patients – human immunoglobulin (NHIG) administered within six days of exposure may be appropriate.
Pharmacists should advise patients with suspected measles to call ahead before visiting their healthcare provider for a PCR test and wear a mask upon leaving home. Suspected cases must remain isolated at home until laboratory testing confirms or excludes measles, avoiding work, school and any public venues.
A notification must be made to the relevant department of health when symptoms are present via the patients’ local public health unit.
Important staff protocols
Fortunately, there were only two members of staff on at the pharmacy including Ms Ngo at the time of the exposure, and neither was infected with measles.
Local PHUs will identify any staff who may have been exposed to a measles case and assess their immunity status, said a spokesperson from the federal Department of Health and Aged Care.
‘Depending on their vaccination history, some staff members may need to be monitored or excluded from work during the infectious period to minimise the risk of further transmission – this could be for a period up to 18 days,’ the spokesperson said. ‘Post-exposure prophylaxis may be required and will be organised by the local PHU.’
With the number of cases currently floating around, pharmacists should ensure that staff are up to date with their vaccinations in advance
All adults born between 1966 and 1992 and who do not have documented evidence of vaccination are eligible for a catch-up vaccine to ensure maximum protection against measles, with the two-dose schedule of the MMR vaccine only being introduced in Australia in 1992.
If you were born during or after 1966 and haven’t had two doses, or you don’t know, get vaccinated.
The MMR vaccine is widely available at GPs and pharmacies.
No Medicare card is required to get a state funded MMR vaccine.
4/6🧵
— Victorian Department of Health (@VicGovDH) April 28, 2025
Should a patient present with a fever and rash, they should be moved out of communal waiting areas and into a dedicated space. If measles is suspected, the patient should be given a disposable, well-sealed mask.




 Symptoms
Symptoms