Why it’s critical to break the flare-up cycle.
Most Australians with asthma have poor control. While there are various reasons for this, when people think of asthma as a condition that waxes and wanes, they are aware flare-ups are easily treated with short-acting beta-agonists (SABAs) and oral corticosteroids (OCS) such as prednisone and prednisolone.
Pharmacists would recognise that many patients can view several courses of OCS a year as a normal part of their treatment. They often perceive it as an acute disease (albeit with flare-ups) rather than a chronic inflammatory condition. And pharmacists would also recognise – just not at the time of dispensing – that every course of OCS, either in long-term administration or repetitive bursts – takes people closer to a total lifetime dose of OCS, which is dangerous.
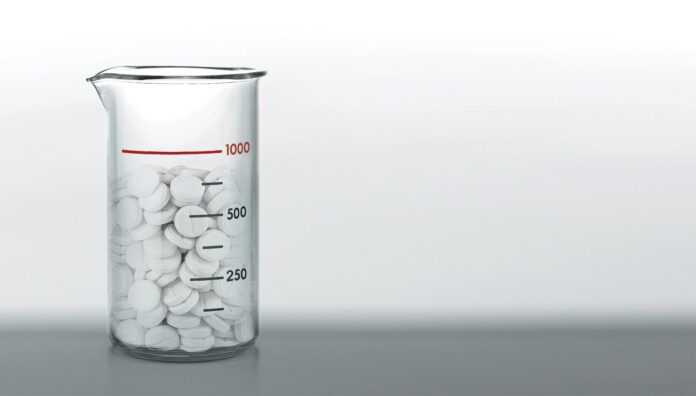
That’s when serious health consequences emerge. That critical lifetime dose – 1,000 mg1 – doesn’t take long to reach. For most adults, just 4–5 courses1 of OCS in their lifetime will get them there, points out credentialed pharmacist Debbie Rigby FPS.
After that threshold, strong evidence shows the risk in adults of severe adverse events increases, including type 2 diabetes, osteoporosis, cardiovascular disease, cataracts, glaucoma, pneumonia and the anxiety and depression associated with any serious disease.2 There is also some evidence of risk for these events in children, according to Ms Rigby.
With oral corticosteroid stewardship, she says that ‘we need to say to people who think nothing of a couple of courses of OCS a year’, that risk of many long-term adverse effects increases once a lifetime exposure to OCS exceeds 1,000 mg prednisolone-equivalent. Instead, all adults and adolescents with asthma, she says, ‘should be routinely using an inhaled corticosteroid (ICS)-containing inhaler to treat the underlying condition, which is chronic inflammation’.
Similarly, repeated COPD and asthma flare-ups can accelerate lung decline and lead to hospitalisation.
‘We know that every time a person with COPD has a flare-up of their condition, they don’t return to where their lung function was prior to that flare-up,’ says Ms Rigby. ‘And every flare-up increases the risk of having another flare-up.’ She has often helped patients with COPD and asthma improve their inhaler technique because there is a significant association between inhaler technique errors and lung condition flare-ups.
A systematic review in 2018 found as many as 90% of patients did not use their inhalers correctly.3
According to the National Asthma Council Australia (NAC), ‘most’ patients with asthma or COPD do not use their inhalers correctly, and most have not had their technique checked or corrected by a health professional.4 Maintenance treatment with poor inhaler technique increases the risk of flare-ups and hospitalisation. And incorrect inhaler technique with ICSs can increase the risk of adverse effects, such as oral thrush and dysphonia.4
Lung Foundation Australia recommends assessing and optimising inhaler device techniques as frequently as possible. Demonstration videos for spacers and inhalers are available on the foundation’s website, including video instructions on the correct technique for Spiromax, Turbuhaler and Reusable Respimat inhalers.5–7
Other pharmacist interventions for COPD and asthma that can help maintain quality of life and reduce the risk of flare-ups include reminders for COVID-19, influenza and pneumococcal disease immunisations⁸ and ensuring patients understand the significant link between allergic rhinitis (hay fever) and asthma.
Rhinitis can trigger a severe asthma flare-up, warns Ms Rigby. Patients with severe asthma should be referred to physicians for eligibility for biologics, she stresses. ‘They are life-changing for some people and underutilised in Australia.’
Case 1
 Debbie Rigby FPS CredPharm (MMR)
Debbie Rigby FPS CredPharm (MMR)
Advanced Practice Pharmacist
Brisbane, Queensland
Ms F, a patient with COPD, lived in a two-storey townhouse and couldn’t climb stairs without sitting down three or four times to rest.
During a Home Medicines Review (HMR), I took the patient through her inhaler technique and found it was ineffective. She wasn’t inhaling hard enough with the inhaler. Dry powder inhalers, which are prescribed for COPD in particular, require a forceful, quick and deep inhalation.
Sometimes patients simply don’t realise how much effort they need to use. Pharmacists can teach patients inhalation techniques to help them use their diaphragm muscles in order to take that necessary quick and deep breath. Patients should stand while inhaling, rather than sitting down.
My advice improved Ms F’s inhaler technique, so we moved on to non-pharmacological matters such as pacing. This might mean a patient stands at the bottom of the stairs and catches her breath before beginning the climb upwards. Pacing is taught in the pulmonary rehabilitation courses offered by many hospitals.
I suggested a 2–4 breathing technique or box breathing – a simple relaxation technique for breathlessness and anxiety, calming the nervous system, reducing stress and improving focus.
The patient sits down and looks at a rectangle shape (e.g. a television screen or window). Looking at the bottom left-hand corner, the eyes move up the short side of the rectangle while breathing in for 2 seconds. Then the eyes move along the top – long side of the rectangle – while exhaling for 4 seconds. I recommended to Ms F, like all my HMR patients, that she this cycle six times, twice a day – or more often if she felt like it.
Returning to Ms F’s townhouse a month later, I saw she could climb the stairs with only one pause, instead of three or four. Ms F was delighted with her progress and her improved quality of life, which was the result of improved inhaler techniques and strategies to help her with her breathlessness.
Case 2
 Alexandra Bradshaw MPS
Alexandra Bradshaw MPS
Community Pharmacist
Priceline Pharmacy George Street
Brisbane, Queensland.
Mr X came into the pharmacy late one Friday afternoon. He was heading to a football game but wanted to get some salbutamol and any advice on assisting with recurrent oral thrush caused by his preventer (Seretide 250/25).
He seemed very deflated struggling to get his asthma under control alongside other conditions – hypertension, diabetes and chronic muscle inflammation due being slightly overweight. He wasn’t a smoker and drank only socially.
Mr X told me he uses his Ventolin puffer often, as the preventer doesn’t seem to help and gives him constant oral thrush. We spoke about his technique and whether or not he uses a spacer, to which he replied sometimes, if he’s at home.
I went through the importance of using his preventer to reduce the inflammation in his lungs and explained that even though the salbutamol gave him short relief, it wasn’t the best at helping him long term. I then showed him the list of inhaler options that are available so he could chat to his doctor about which ones may be suitable for him that may not create oral thrush.
When I showed Mr X this list, his eyes lit up. There were options and a possible solution to his ongoing ineffective treatment and major adverse effect.
We spoke about options for rinsing his mouth out to help reduce the incidence of oral thrush. These included water, salt and water, and an antibacterial mouthwash, which he chose to try. He left ready for the game, feeling like he had more control over his condition than when he walked in.
Even though Mr X was seeing his GP and a specialist, it had been some time since these simple steps were explained to him and more treatment options were put forward.
It’s important to just arm people with knowledge so they can make a joint decision with their healthcare provider about managing their particular conditions.
References
- Price DB, Trudo F, Voorham J, et al. Averse outcomes from initiation of systemic corticosteroids for asthma: long-term observational study. J Asthma Allergy 2018;11:193–204.
- Hancock KL, Bosnic-Anticevich S, Blakey JD, et al. Characterisation of the Australian adult population living with asthma: severe – exacerbation frequency, long-term OCS use and adverse effects. Pragmat Obs Res 2022;13:43–58.
- Usmani OS, Lavorini F, Marshall J, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. BMC Open Respir Res 2018;19(10). Epub 2018 Jan 16. At: https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-017-0710-y
- National Asthma Council Australia. Inhaler technique for people with asthma or COPD. 2025. At: www.nationalasthma.org.au/living-with-asthma/resources/health-professionals/information-paper/hp-inhaler-technique-for-people-with-asthma-or-copd
- Lung Foundation Australia. How to use a Spiromax®: video. At: https://lungfoundation.com.au/resources/inhaler-device-technique-spiromax/
- Lung Foundation Australia. How to use a Turbuhaler®: video. At: https://lungfoundation.com.au/resources/inhaler-device-technique-turbuhaler/
- Lung Foundation Australia. How to use a Reuseable Respimat®: video. At: https://lungfoundation.com.au/resources/inhaler-device-technique-respimat-2/
- Healthline. Steroids for COPD. 2025. At: www.healthline.com/health/copd/steroids#inhaled-steroids




 Deborah Williams at the Chemist Warehouse Australian Open pop-up pharmacy[/caption]
Deborah Williams at the Chemist Warehouse Australian Open pop-up pharmacy[/caption]


 Rebecca Davies[/caption]
Rebecca Davies[/caption]

 Professor Clare Collins[/caption]
Professor Clare Collins[/caption]
 Associate Professor Trevor Steward[/caption]
Associate Professor Trevor Steward[/caption]