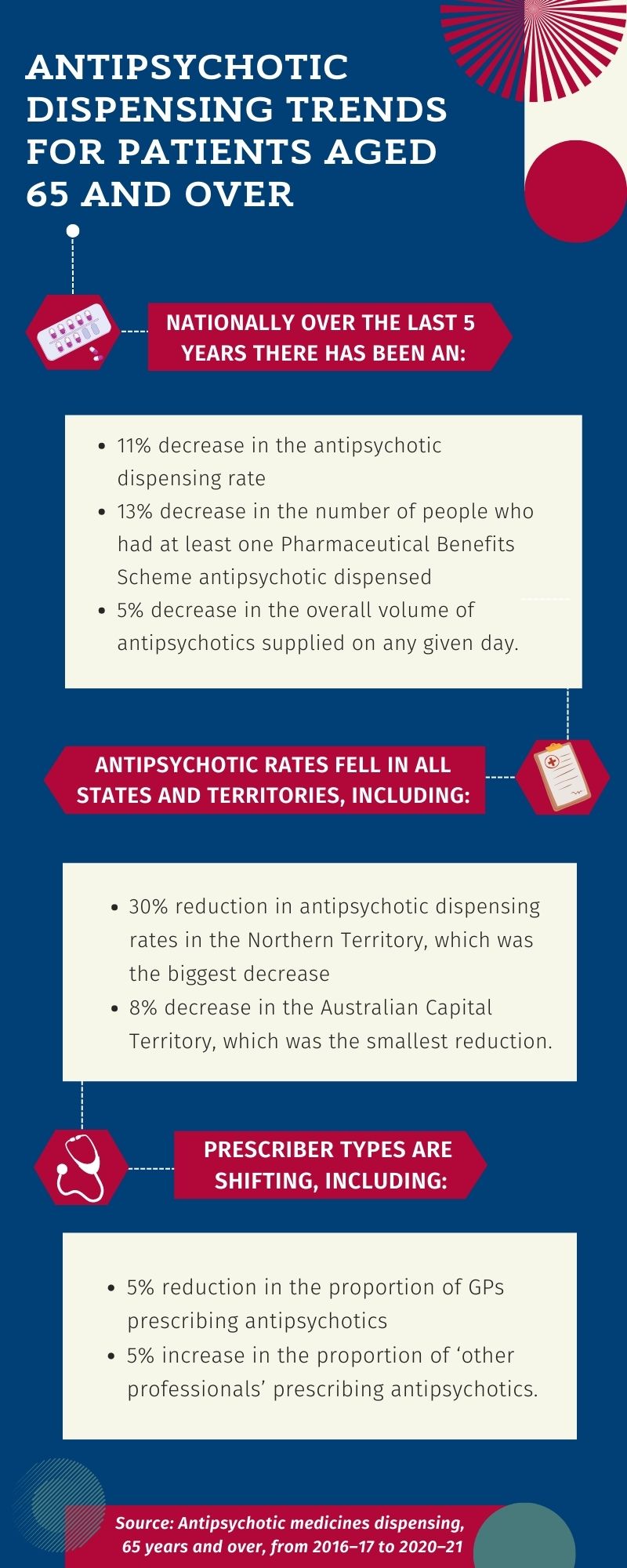
A new report by the Australian Commission on Safety and Quality in Health Care revealed that there has been a reduction in antipsychotic dispensing in the past 5 years.
The Antipsychotic medicines dispensing, 65 years and over, from 2016–17 to 2020–21 report found there was an 11% decrease in the rate of antipsychotic dispensing for this patient cohort, along with a 5% reduction in the overall volume of antipsychotic medicines provided to older patients.
This report also unearthed geographical variation in the rate of antipsychotic dispensing, with higher rates in urban locales than in regional areas. Dispensing rates also increased for socioeconomically disadvantaged groups each year of the reporting period.
It has been 18 months since the Final Report of the Royal Commission into Aged Care Quality and Safety was tabled in federal Parliament in March last year, which recommended a range of measures to minimise antipsychotic prescribing for the purposes of chemical restraint. These included prescribing restrictions, education, quality improvement programs and, effective from 1 July 2021, changes to aged care legislation.
Two aged care pharmacists explained to Australian Pharmacist how some of these initiatives, among others, are making an impact.
Mandatory reporting and recorded diagnosis
Amelia Wood MPS, who has been working at Longridge Aged Care in Naracoorte, South Australia for 3.5 years, said there has been a pronounced change in the management of antipsychotic medicines since the royal commission recommendations were implemented.
What was once a ‘set and forget’ approach is now a process of careful review – complete with mandatory and self-managed check-ins.
‘We do a review every month of all antipsychotics, and I’ll pop in [residents’] notes how long they have been on it and why they’re on it,’ she said.
‘Then I follow up every 12 weeks to [check] that it’s still a reasonable thing to be prescribing.’
Legislation also dictates all patients taking an antipsychotic now need to have a diagnosis that warrants prescribing of the medicine, Ms Wood said.
This reform was designed to limit antipsychotic prescribing for behavioural and psychological symptoms of dementia (BPSD), with emerging evidence revealing that non-pharmacological strategies, including social contact, environmental changes, psychological interventions, and meaningful activities are more effective.
 Deprescribing more commonplace
Deprescribing more commonplace
In the last 2 years, Ms Wood said successful deprescribing of antipsychotics has increased, which typically begins with a trial.
‘There were a lot of people who were on antipsychotics when I first started, and now are not, and they’re doing quite well,’ she said.
For example, one resident with a mood disorder, who came to Longridge 5 years ago, was put on antipsychotics from the get-go. The resident had been experiencing drowsiness during the day, with Ms Wood frequently pushing for a deprescribing trial.
‘It was very unclear why she was put on antipsychotics in the first place, I think it was just to cover all bases,’ she said.
The resident was successfully deprescribed from antipsychotics following the trial, and no longer experiences drowsiness. She now takes an antidepressant to manage her mood disorder.
However, when the first trial doesn’t succeed there are still deprescribing opportunities further down the line – particularly if the person’s circumstances change.
This was the case with another resident, who was put on antipsychotics 12 months ago after experiencing frequent ‘sundowning’ – pronounced agitation, aggression and confusion that typically comes on in the late afternoon.
‘About 6 months ago, we trialled deprescribing and that didn’t quite work. She was still getting a bit agitated in the afternoon,’ Ms Wood said. ‘But recently, her health has gone downhill so we tried it again.’
This time, the resident was successfully deprescribed from risperidone, and now also takes an antidepressant to manage her symptoms.
Antidepressant prescribing on the rise
Along with changes to antipsychotic prescribing, there has been a significant upswing in antidepressant prescribing over the last couple of years, Ms Wood said.
Her next project at Longridge is investigating the reason behind the jump, which could be down to several factors.
‘[It could be] because of COVID-19 and not being able to see people and socialise, or antidepressants might be used instead of antipsychotics because of the better adverse effect profile,’ she said.
‘[Antidepressants] are also used for pain, as an adjunct, so opioids are not increased.’
Educating prescribers
Since the evidence of widespread use of antipsychotics for chemical restraint was revealed during the royal commission (2018–2021), doctors are increasingly aware their prescribing practices are subject to review, and they have a greater understanding of the need for caution, Ms Wood said.
But pharmacists have also played a big role in changing antipsychotic prescribing patterns through education.
‘There was one doctor who was from the old school of prescribing practices. I had a lot of one-on-one informal chats with her, and she eventually came around and did a bit of deprescribing,’ she said.
In fact, all new doctors who start at Longridge are open to trialling deprescribing, with Ms Wood broaching the topic as soon as they come on board.
‘[When they start] I introduce myself over email first, explaining what I do, and if they want to chat they can,’ she said.
‘They come to the facility once a month, so I’m able to catch up with them and discuss about anyone who [has concerns].’
Ms Wood is also instrumental in keeping doctors informed about the specific requirements for antipsychotic prescribing.
A deep dive into antipsychotic use
Sharon Doolan MPS, a Wollongong-based consultant pharmacist who works across several Residential Aged Care Facilities (RACFs), said that in her experience there are many initiatives contributing to reduced antipsychotic prescribing.
This includes Residential Medication Management Reviews (RMMRs), which help to ascertain the use, indication, adverse effects, and risk of using antipsychotics.
Then there are RMMR follow-ups, introduced on 21 April 2020, which can be undertaken within 9 months of an RMMR.

‘[Follow-ups] allow for additional medication review, specifically addressing the recommendations from the initial review, which may have contributed to antipsychotic use reduction in more recent times,’ she said.
Regular Medication Advisory Committee (MAC) meetings also provide an opportunity to identify the overall usage of antipsychotics in an RACF.
‘[We] look at the prescribing, falls, [and] hospitalisation statistics, so we can marry up any connection with antipsychotic prescribing and the risks that residents may be experiencing,’ Ms Doolan said.
MAC meetings are helpful for ensuring patients’ documented diagnoses are not to address BPSD, which may constitute chemical restraint.
‘We look at every resident’s [use] of antipsychotics and the percentages of antipsychotic prescribing, whether regular use or pro re nata, and which one was more likely to be prescribed,’ Ms Doolan said.
Clinical governance
Governance is another area pharmacists can get involved in to improve rates of antipsychotic use, Ms Doolan said.
‘Having a better-informed RACF Board [through] reportable information can lead to a discussion about prescribing habits with antipsychotic use,’ she said.
Embedding a clinical governance committee within the Board is also beneficial.
‘The [clinical governance committee] presents their data quarterly and has to enter the specific use of antipsychotics, falls [incidence] and other information [which is] presented as an overall facility report.’
Furthermore, the National Aged Care Mandatory Quality Indicators Program, which was updated on 1 July 2021 to include new indicators, means RACFs need to collect data and report on:
- pressure injuries
- physical restraint
- unplanned weight loss
- falls and major injury
- medication management, including polypharmacy and antipsychotics.
‘The data submitted are in percentage form generated from the review of antipsychotic use for every resident in the facility at the end of each quarter,’ Ms Doolan said.
‘This means that over time, trends on the use of antipsychotic medications can be observed and addressed.’




 ‘We’re increasingly seeing incidents where alert fatigue has been identified as a contributing factor. It’s not that there wasn’t an alert in place, but that it was lost among the other alerts the clinician saw,’ Prof Baysari says.
‘We’re increasingly seeing incidents where alert fatigue has been identified as a contributing factor. It’s not that there wasn’t an alert in place, but that it was lost among the other alerts the clinician saw,’ Prof Baysari says.


 Beyond the arrhythmia, AF often signals broader pathological processes that impair cardiac function and reduce quality of life and life expectancy.5 Many of these conditions are closely linked to social determinants of health, disproportionately affecting populations with socioeconomic disadvantage. Effective AF management requires addressing both the arrhythmia and its underlying contributors.4
Beyond the arrhythmia, AF often signals broader pathological processes that impair cardiac function and reduce quality of life and life expectancy.5 Many of these conditions are closely linked to social determinants of health, disproportionately affecting populations with socioeconomic disadvantage. Effective AF management requires addressing both the arrhythmia and its underlying contributors.4  C – Comorbidity and risk factor management
C – Comorbidity and risk factor management Warfarin
Warfarin




