Neuropathic pain is defined as ‘pain caused by a lesion or disease of the somatosensory nervous system’.1
It is associated with impaired quality of life. Around 7–8% of adults have chronic pain with neuropathic characteristics. A quarter of people with diabetes and 35% of people with HIV have neuropathic pain.2
The management of neuropathic pain can be challenging; it is often poorly treated. There are several options for drug treatment as part of an overall approach to improve patients’ quality of life.3
One complementary medicine, capsaicin, the active constituent of the capsicum species, has shown positive results in reducing certain types of neuropathic pain.
Capsicum/Capsaicin
What is it?
Capsaicin is the active constituent of capsicum species – Capsicum frutescens, C. annuum or other species from the Solanaceae plant family. It is responsible for the irritant effects of capsicum.4 Studies have trialled topical capsaicin for the treatment of neuropathic pain. Creams, ointments and patches/plasters containing capsicum and creams containing capsaicin are available in Australia.
Evidence for neuropathic pain
A 2014 Cochrane review of five RCTs (n = 956) concluded that C. frutescens cream or plaster reduces chronic lower back pain more than placebo.5
A 2014 systematic review of three RCTs found that topical capsaicin 0.075% resulted in statistically signi‑ cant reductions in diabetic neuropathic pain within 3 months of treatment.6
A 2017 Cochrane review assessed a single 30–90-minute application of an 8% capsaicin skin patch in moderate to severe chronic post-herpetic neuralgia (four RCTs, n = 1272), peripheral diabetic neuropathy (one RCT, n = 369), HIV neuropathy (two RCTs, n = 801) and persistent pain following inguinal hernia repair (one RCT, n = 46). The reviewers concluded that there was moderate-quality evidence that high-concentration (8%) capsaicin patches give at least moderate pain relief to a small number of people with post-herpetic neuralgia, and very low quality evidence that it benefits those with HIV neuropathy or peripheral diabetic neuropathy.7
A 2017 systematic review of six RCTs (n = 1449) investigated the efficacy of high- and low-concentration capsaicin creams and patches in chronic post-herpetic neuralgia. The results of all studies were in favour of capsaicin treatment, but the statistical significance of the results could not be determined.8
Suggested counselling advice
Capsaicin cream can take 14 days or more of daily use to relieve pain. If the pain worsens, or does not improve after 4 weeks of use, patients are advised to stop using the cream and see a doctor.9
The cream should be massaged in a thin layer into the affected area three or four times daily. Use gloves or wash hands well after application (unless treating the hands). Make sure the cream does not make contact with your eyes, mouth or genitals; the inside of your nose; or broken or irritated skin.9
Cream or patches can cause a burning feeling, redness and irritation. The burning feeling should decrease after 2 weeks of use.6,7 If the cream or patch causes pain, swelling or blistering, patients should stop using it and see a doctor immediately.4,9
The risk and intensity of side effects increases as the capsicum/capsaicin dose or concentration increases.
Dose
Topical capsaicin cream 0.025–0.075% w/w three or four times daily has been used for musculoskeletal and neuropathic pain. Other forms (e.g. patches, plasters) and higher-strength preparations have also been used.9,10
Learn more
For more evidence-based information about these and other complementary medicines – including clinical notes on adverse effects, contraindications and interactions, as well as full references, refer to the Australian Pharmaceutical Formulary and Handbook 24th edition (APF24). APF is available in print or digital format. Digital APF is available at apf.psa.org.au (subscription required).
References
- International Association for the Study of Pain. IASP Terminology. Pain terms. Neuropathic pain. 2017 At: iasp-pain.org/Education/Content.aspx?ItemNumber=1698#Neuropathicpain
- International Association for the Study of Pain. Epidemiology of neuropathic pain: how common is neuropathic pain, and what is its impact? Washington: IASP; 2014. http://s3.amazonaws.com/rdcms-iasp/files/production/public/AM/Images/GYAP/Epidemiology%20of%20Neuropathic%20Pain.pdf
- Veterans Mates Therapeutic Brief 35. Topic 35: Managing neuropathic pain: a stepwise approach. 2013. At: veteransmates.net.au
- Memorial Sloan Kettering Cancer Center. About herbs, botanicals and other products. 2017. At: mskcc.org/cancer-care/diagnosis-treatment/symptom-management/integrative-medicine/herbs
- Oltean H, Robbins C, van-Tulder MW, et al. Herbal medicine for low-back pain. Cochrane Database of Systematic Reviews 2014, Issue 12. At: https://www.ncbi.nlm.nih.gov/pubmed/25536022
- Griebeler ML, Morey-Vargas OL, Brito JP, et al. Pharmacologic interventions for painful diabetic neuropathy: an umbrella systematic review and comparative effectiveness network meta-analysis. Ann Intern Med 2014;161(9):639–49. At: https://www.ncbi.nlm.nih.gov/pubmed/25364885
- Derry S, Rice AS, Cole P, et al. Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database of Systematic Reviews 2017, Issue 1. At: https://www.ncbi.nlm.nih.gov/pubmed/23450576
- Yong YL, Tan LT, Ming LC, et al. The effectiveness and safety of topical capsaicin in postherpetic neuralgia: a systematic review and meta-analysis. Front Pharmacol 2016;7:538. At: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5222862/
- eMIMS cloud. Sydney: MIMS Australia; 2017. At: http://www.mims.com.au/index.php/products/emims
- Derry S, Sven-Rice A, Cole P, et al. Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database of Systematic Reviews 2013, Issue 2. At: https://www.ncbi.nlm.nih.gov/pubmed/23450576




 ‘We’re increasingly seeing incidents where alert fatigue has been identified as a contributing factor. It’s not that there wasn’t an alert in place, but that it was lost among the other alerts the clinician saw,’ Prof Baysari says.
‘We’re increasingly seeing incidents where alert fatigue has been identified as a contributing factor. It’s not that there wasn’t an alert in place, but that it was lost among the other alerts the clinician saw,’ Prof Baysari says.

 Beyond the arrhythmia, AF often signals broader pathological processes that impair cardiac function and reduce quality of life and life expectancy.5 Many of these conditions are closely linked to social determinants of health, disproportionately affecting populations with socioeconomic disadvantage. Effective AF management requires addressing both the arrhythmia and its underlying contributors.4
Beyond the arrhythmia, AF often signals broader pathological processes that impair cardiac function and reduce quality of life and life expectancy.5 Many of these conditions are closely linked to social determinants of health, disproportionately affecting populations with socioeconomic disadvantage. Effective AF management requires addressing both the arrhythmia and its underlying contributors.4  C – Comorbidity and risk factor management
C – Comorbidity and risk factor management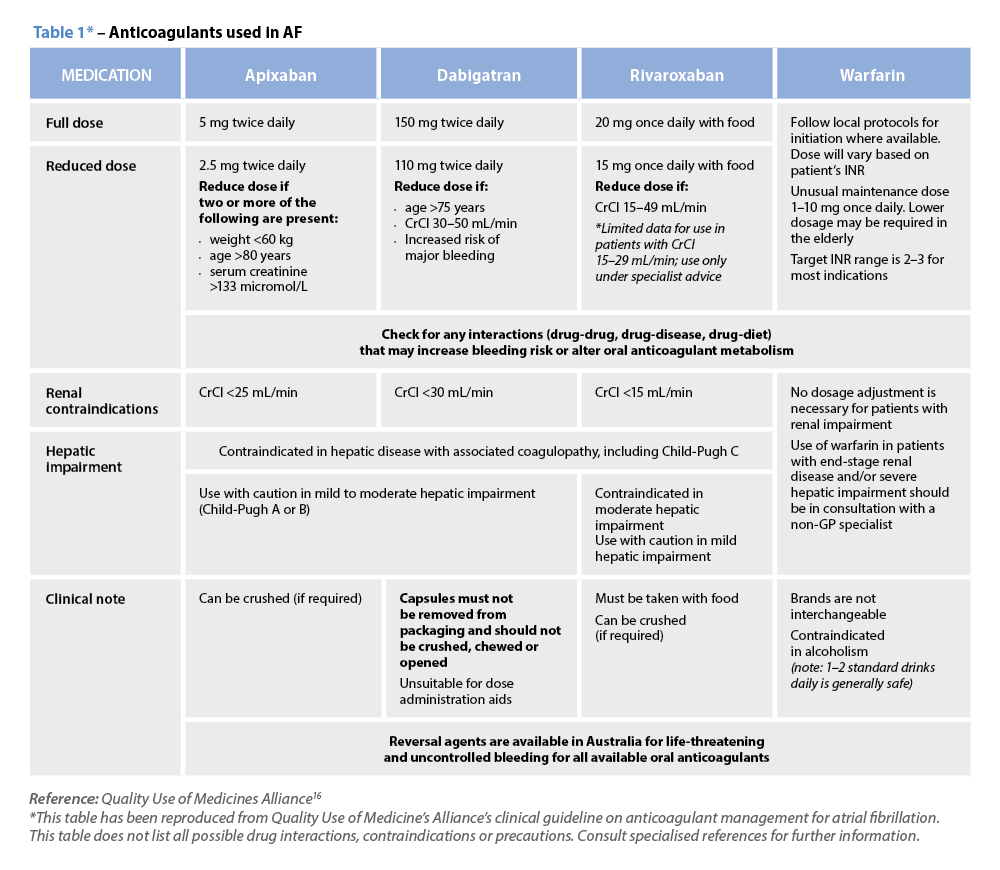 Warfarin
Warfarin







