Many women in their mid-to-late forties are quick to accept headaches, irritability and memory loss as an unavoidable part of stressful lives. But new research suggests that they might be suffering from perimenopausal depression – an under-researched condition where pharmacists can play a valuable role.
For the past decade a team from Monash Alfred Psychiatry Research Centre – led by the centre’s Director, Professor Jayashri Kulkarni – have compiled data from women going through the menopause transition to better understand the impact this period has on women’s psychological health.
Perimenopause is defined by WHO as ‘the time immediately preceding the menopause, beginning with endocrine, biologic and clinical changes, and ending a year after the final menstrual period.’1
Professor Kulkarni noted the high rates of suicide in women aged between 45-492 , and suggests that they should ‘alert us to think about contributing factors, including biological changes in the gonadal hormones associated with the transition to menopause as well as social and psychological stresses in the midlife period.’
The symptoms
There are a range of psychological and somatic symptoms in perimenopausal depression that are also seen in ‘typical depression,’ which often leads to incorrect diagnoses and treatment.
But Professor Kulkarni said many of that the psychological symptoms of the condition are different to what you would normally see in major depression in men or younger women. Perimenopausal depression can often fluctuate in severity where irritability, paranoia and memory loss are often prominent compared to major depression.
‘We see many women who say “I don’t know what’s going on, I suddenly can’t remember things such as phone numbers, shopping lists and so on”,’ she said.
In addition to psychological symptoms, many women also experience somatic symptoms.
‘There’s often joint or muscle aches and pains, and frequent headaches. There are different aches and pains that occur that don’t really fit within the pattern of any particular pathology. Nonetheless, it adversely impacts a person’s capacity to function.’
Unlike other forms of depression, which are usually the result of an interaction between a genetic predisposition and environmental triggers, Professor Kulkarni and her team have found that perimenopausal depression is primarily the result of hormonal changes.
This means that hormonal treatment can be highly effective, but a lack of information about the condition can make an accurate diagnosis and treatment difficult.
‘One of the problems we have is that many women get started on SSRI’s or an SNRI, which might make a little bit of a difference but won’t make a complete difference to the symptoms. The patient’s depression might then be considered treatment resistant depression and there’s a terrible cycle through the different antidepressants or combinations of medications, each with their own side effects. Patients will get this sort of half response, but not a great response,’ Professor Kulkarni explained.
She said healthcare professionals such as pharmacists can help women around the age of 45 years and older to recognise that the sudden development of any of these symptoms can be a result of hormonal changes. These changes will occur well before physical changes and should be thought of as the trigger for the symptoms, which will then inform treatment choice .
How pharmacists can help
Professor Kulkarni suggests that pharmacists might have a key role to play in treating perimenopausal depression, especially given the reluctance of many women to seek help from their doctors.
‘Pharmacists could alert patients to the symptoms of perimenopausal depression and advise them to seek help when appropriate,’ she said. ‘Given their accessibility to patients, pharmacists can refer patients to other healthcare professionals who can prescribe hormone replacement therapy.’
In her recent study, Professor Kulkarni suggested a range of treatments.
‘Effective treatments include tibolone, a synthetic steroid with a mixed hormonal profile, and bioidentical hormones, which are compounds synthesised to resemble ovarian hormones. Bioidentical hormones are not recommended by the International Menopause Society due to the limited available safety and dosing data,’ the study read.3
Professor Kulkarnii said that perimenopausal depression is a relatively new concept and that ultimately, education and awareness are essential for healthcare professionals.
‘When you talk about menopause, everyone thinks hot flushes. That’s what most of the community’s education centres on. But all women go through menopause and a significant number struggle with the mental health aspect of it.’
References
1-3: Kulkarni J. Perimenopausal depression – an under-recognised entity. Aust Prescr 2018;41(6):183–5. At: https://www.nps.org.au/australian-prescriber/articles/perimenopausal-depression-an-under-recognised-entity




 ‘We’re increasingly seeing incidents where alert fatigue has been identified as a contributing factor. It’s not that there wasn’t an alert in place, but that it was lost among the other alerts the clinician saw,’ Prof Baysari says.
‘We’re increasingly seeing incidents where alert fatigue has been identified as a contributing factor. It’s not that there wasn’t an alert in place, but that it was lost among the other alerts the clinician saw,’ Prof Baysari says.

 Beyond the arrhythmia, AF often signals broader pathological processes that impair cardiac function and reduce quality of life and life expectancy.5 Many of these conditions are closely linked to social determinants of health, disproportionately affecting populations with socioeconomic disadvantage. Effective AF management requires addressing both the arrhythmia and its underlying contributors.4
Beyond the arrhythmia, AF often signals broader pathological processes that impair cardiac function and reduce quality of life and life expectancy.5 Many of these conditions are closely linked to social determinants of health, disproportionately affecting populations with socioeconomic disadvantage. Effective AF management requires addressing both the arrhythmia and its underlying contributors.4  C – Comorbidity and risk factor management
C – Comorbidity and risk factor management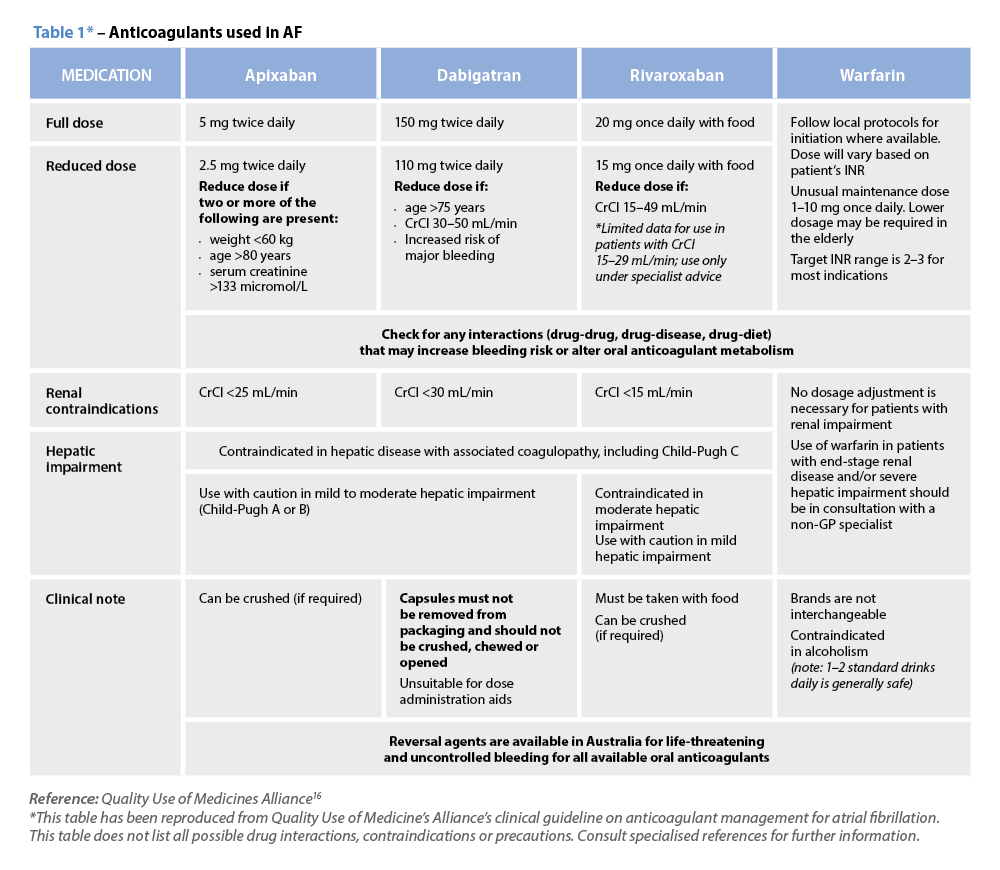 Warfarin
Warfarin







