For Australians living with chronic wounds, pharmacy wound clinics can provide an accessible journey to healing.
From venous leg ulcers to diabetic foot ulcers, arterial ulcers and pressure injuries, more than 420,000 Australians experience a chronic wound every year.1 Wounds Australia describes this as a ‘hidden epidemic’ that costs the nation’s health and aged care budgets more than $3 billion annually.1 For the people who experience them, chronic wounds can have a profound impact on daily life.1
A chronic wound is one that has not healed within 3 months.2 While healing is possible, the right treatment at the right time is vital. But correct diagnoses, treatment pathways and consumables are not always easily accessible. Cost can be a major barrier, with wound consumables or the products necessary for healing often costing patients thousands of dollars.1
Beginning this year, the Australian Government’s provision of $47.8 million over the next 5 years is expected to improve chronic wound treatment through the Chronic Wound Consumables Scheme. This will offer subsidised wound consumables to eligible patients, including those with diabetes aged 65 years or older, or Aboriginal or Torres Strait Islander Australians older than 50 years.3 The scheme will also provide healthcare professionals with education and training on chronic wound management.

Pharmacies are often the first port of call for patients dealing with a wound, and most chronic wounds are managed in the community, rather than the hospital setting. By upskilling in chronic wound management, pharmacists have the opportunity to expand their practice, help their patients and take the pressure off secondary and tertiary care facilities.
Understanding different types of chronic wounds and how to treat them is vital. So, too, is multidisciplinary collaboration, says Samantha Kourtis, a wound care specialist and managing partner at Capital Chemist Charnwood in the ACT.
‘A pharmacist cannot fix a chronic wound by themselves,’ she says.
‘There will be an underlying aetiology as to why a wound is chronic, and addressing that will often require close collaboration with people like GPs, high-risk and tissue-viability nurses, dietitians and infectious disease specialists. When all these people have started to input, that’s when we can begin to heal the wound. So, you need to know what a chronic wound is, but also your part in the puzzle.’
AP spoke with Ms Kourtis and experienced wound care pharmacist Karen Carter FPS about how they approach managing chronic wounds.
Case 1
 Karen Carter FPS Owner and pharmacist, Carter’s Pharmacy, Gunnedah, NSW
Karen Carter FPS Owner and pharmacist, Carter’s Pharmacy, Gunnedah, NSW
One of our regular patients, Mrs J, is a 68-year-old female with a diabetic foot ulcer. She previously had osteomyelitis in her other foot, which was amputated.
We’re working with the local high-risk foot services clinic and the local major hospital to help prevent this from happening again.
Mrs J lives 45 minutes away from Gunnedah and gets transport into town through the NDIS three times a week. We dress the wound for her while she’s here. Because she knows us, she trusts us and is comfortable with us changing the dressing. We charge a fee for the service but the dressings are supplied.
First, we unwrap the previous dressing and assess how the wound has changed since the last time we saw it. We have a wound assessment template we fill in, and we take photos using an iPad that can be shared with other health professionals. At the moment, once the wound is cleaned, we use a low-adherent dressing pad and then wrap it up. In the past, Mrs J has used dressings that contained silver, but we’re following the direction of the foot services clinic. There is also a suggestion of using something like cadexomer-iodine in future.
Wound care is about more than just the wound. Psychological stress can have an effect on healing, as can nutrition and how well Mrs J’s diabetes is controlled. We need to ensure she’s not anaemic, because the oxygen-carrying capacity of the blood needs to be good, so that oxygen can get to the wound. We’ve had conversations about ensuring she’s eating food that is high in protein, things like scrambled eggs.
Mrs J smokes and doesn’t like the idea of stopping cigarettes. I’ve learnt not to be so forthcoming – I was quite blunt the first time we spoke about it. I understand that it’s her choice, but I’m hoping we can chip away at that over time. At the moment, she has some independence. She’s still able to manage things like using a wheelchair and showering. But if the other foot goes, that independence will really change. It makes ensuring the wound is cared for properly even more important.
Case 2

Samatha Kourtis (she/her) Managing Partner and pharmacist, capital Chemist Charnwood, ACT
I first met Mr S, a man in his 60s, about 10 years ago after referral from ACT community nursing with a prescription for class 2 compression.
He’d had a venous leg ulcer that was healed by the nurses who had wrapped him in a class 3 compression bandage. In the ACT, chronic wound care for such a patient is funded until the wound is healed, but they must source their own compression.
Although much time and resources are consumed during the processes of healing venous leg ulcers (VLUs),4 unfortunately, once healed, as many as 60–70% of patients suffer a recurrence. The VLU guidelines recommend medical-grade graduation compression as a tool to address venous insufficiency and prevent recurrence.5
Unfortunately, Mr S disliked wearing compression garments. Six years later, he came into the pharmacy with a skin tear that was on the edge of becoming chronic. It wasn’t ulcerated yet, but it wasn’t healing because he wasn’t wearing the compression garment. Due to my background in wound care, I suggested an appropriate dressing for the wound that was waterproof, bacteria proof and vapour-permeable.
Mr S came in weekly so we could apply the dressing. He decided to wear his compression garments again, and thus we were able to heal the skin tears, which had been developing for about 10 weeks. I’m passionate about this type of prevention.
Another patient was a woman in her 90s with congestive heart failure and coming to the end of her life. Her daughter saw me and explained she had a pea-sized melanoma on the back of her calf that had ulcerated. It was leaking 50–100 mL of fluid each day – with a smell. This stopped her from leaving the house and meant she had to change her bedding constantly.
Her daughter tried everything to soak up the fluid, from tea bags to incontinence pads – anything to help her mum enjoy the rest of her life. An alginate dressing with silver in it was recommended. Alginate absorbs a phenomenal amount of fluid, so it is useful for very wet wounds, and silver helps reduce the microbial load and stop infection. A 20 x 10 cm sheet of this alginate costs $80. We bought the dressing. The daughter cut it into strips that she then concertina folded and put on top of the melanoma, covering it with a high-absorbent foam.
The dressings lasted 48–72 hours. Her mum could go out to a cafe, or go to sleep at night and not wake up wet. It vastly improved her quality of life. Her daughter did this for the rest of her mum’s life.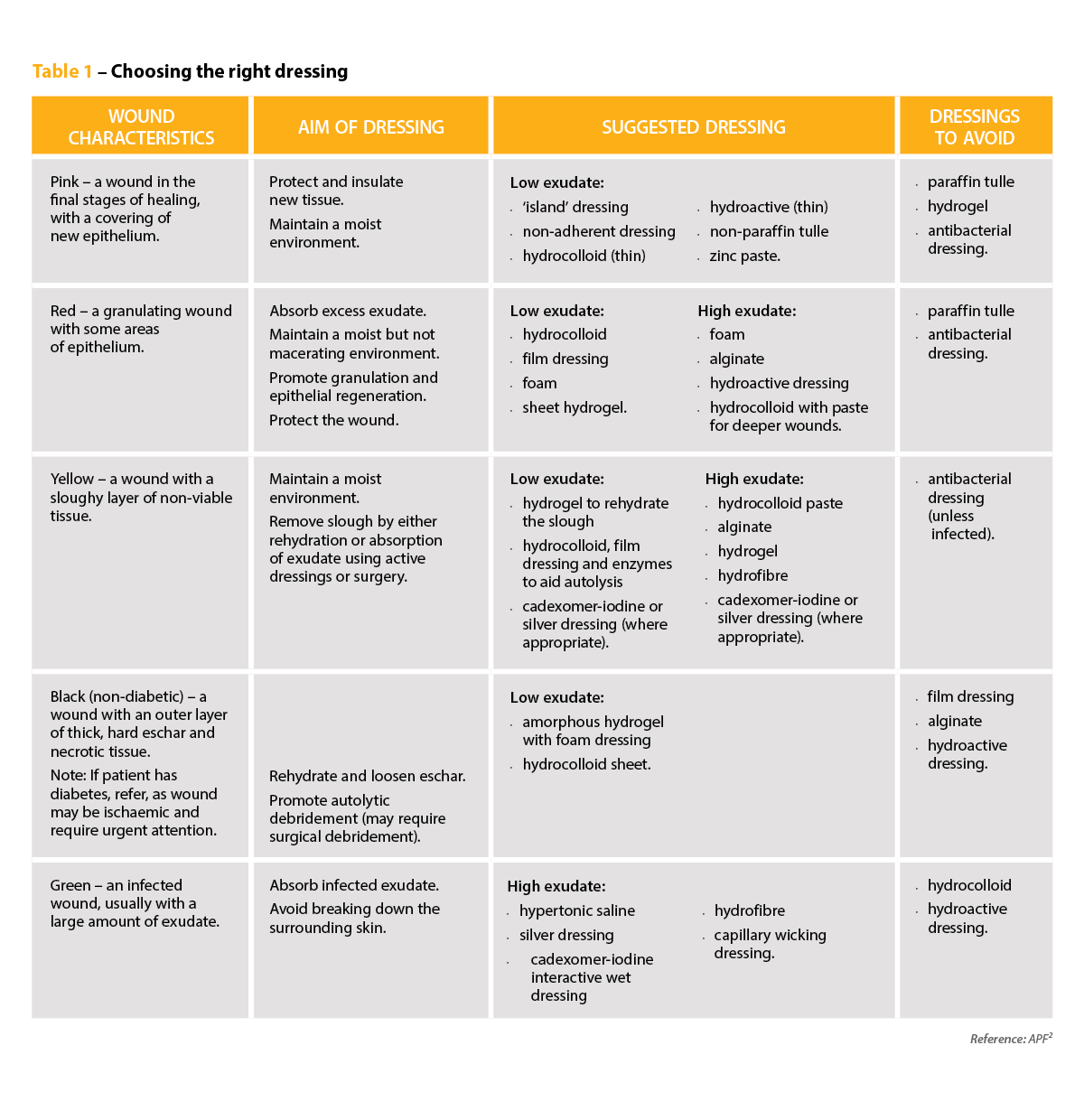
References
- Wounds Australia. Pre-budget submission to fight Australia’s chronic wound epidemic. At: treasury.gov.au/sites/default/files/2022-03/258735_wounds_australia.pdf
- Services Australia. Budget 2023–24: strengthening Medicare. 2023. At: www.servicesaustralia.gov.au/sites/default/files/2023-05/budget-2023-24-may-health-and-disability-12.pdf
- Australian Pharmaceutical Formulary. Wound management. PSA. 2023. At: apf.psa.org.au/wound-management/wound-management
- Finlayson KJ, Edwards HE, Courtney MD. Venous leg ulcer recurrence: deciphering long-term patient adherence to preventive treatments and activities. Wound Pract Res 2014; 22(2): 91–7.
- New Zealand Would Care Society. Australian and New Zealand clinical practice guideline for prevention and management of venous leg ulcers. 2011. At: www.nzwcs.org.nz/images/luag/2011_awma_vlug.pdf



 John Jones MPS, pharmacist immuniser and owner of My Community Pharmacy Shortland in Newcastle, NSW[/caption]
John Jones MPS, pharmacist immuniser and owner of My Community Pharmacy Shortland in Newcastle, NSW[/caption]


 Debbie Rigby FPS explaining how to correctly use different inhaler devices[/caption]
Debbie Rigby FPS explaining how to correctly use different inhaler devices[/caption]




 Professor Sepehr Shakib[/caption]
Professor Sepehr Shakib[/caption]

 Lee McLennan MPS[/caption]
Lee McLennan MPS[/caption]
 Dr Natalie Soulsby FPS, Adv Prac Pharm[/caption]
Dr Natalie Soulsby FPS, Adv Prac Pharm[/caption]
 Joanne Gross MPS[/caption]
Joanne Gross MPS[/caption]








