This national resource supports frontline assessment, management and prompt referral of burn injuries.
Community pharmacists are often the first point of contact for health concerns and public health initiatives, including burns, said Rebecca Schrale, Burns Nurse Practitioner at the Royal Hobart Hospital’s Burns Unit and Australian and New Zealand Burn Association (ANZBA) Burns Prevention Representative for Tasmania.
‘[So] community pharmacists are in a unique position to provide education on initial first aid, referral and wound care,’ she said. ‘They also have an important role in prevention of burn injuries, educating the community and reducing risk.’
To that end, ANZBA, PSA and the National Australian Pharmacy Students’ Association (NAPSA) collaborated to develop guidelines specifically for pharmacists to assist with the assessment and management of burns.
Australian Pharmacist investigates what pharmacists should look out for and how to manage and refer burns appropriately.
What burns do community pharmacists typically encounter?
The full spectrum – from minor to severe, said PSA Tasmania State Manager Dr Ella van Tienen FPS.
‘A lot of it is advice for minor sunburn or small burns,’ she said. ‘But you do get some more serious burns when people aren’t sure what to do with them, or whether they’re serious enough to [require further attention].’
Burns are more likely to occur out of hours, such as on weekends and public holidays – particularly among children – when general practices are typically closed.
‘That’s when kids are home,’ Dr van Tienen added.
Common causes of burns in children include hot water scalds due to access to kettles or stove tops.
‘Teenagers who are newly independent and off at the beach on their own, also present with blistering sunburn,’ she said.
What impact do burns have on the community?
It’s important to remember that even minor burns can have long-term effects on the patient in regard to range of movement, function and the look and feel of the scar, Ms Schrale said.
‘All burn injuries – whether large or small can have a psychological effect on the individual and their family,’ she said. ‘And it’s imperative that patients are referred to burns clinicians in a timely manner.’
Deep burn injuries will result in scarring and could restrict the function of the area that is affected.
‘Pharmacies are often open after hours and on weekends so again they provide clients and their families with timely advice, education and support,’ Ms Schrale said.
What does the burns resource involve?
The new Pharmacists Advisory Card and A3 Poster are new iterations of an old resource, Dr van Tienen said.
‘The original resource had been around for many years, and it needed to be updated,’ she said.
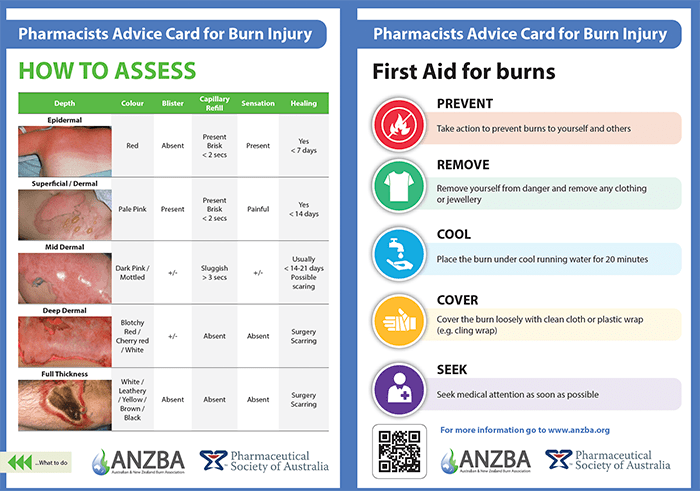
The refreshed burns advisory resource provides pharmacists with up-to-date information on Burns First Aid, and assessment – including burn depth, assessment and minor burn wound care, Ms Schrale said.
‘With this knowledge they are equipped to then follow the ANZBA referral guidelines, highlighting who requires discussion or referral to primary [care] or the local emergency department (ED),’ she said. ‘The updated card ensures the messaging is consistent across pharmacies, community health, primary care and EDs nationally.’
What new information is included?
The new version of the card focuses on information that will assist in early assessment, management and referral of minor burns, Ms Schrale said.
‘It also provides simple and consistent messaging on wound care and medical emergencies – such as large surface area burns, airway burns, circumferential burns and infection,’ she said.
‘The other new addition is the inclusion of information on burns scar management based on evidence-based practice and encouraging referral for any patient who sustains a scar from a burn injury.’
How can the burns resource be used in practice?
Let’s say a parent presents to the pharmacy with a child who has sustained a burn after accidentally knocking over a pot of boiling water while cooking pasta on the stove.
‘If the child has a small [dermal] burn that’s not significantly blistered, the pharmacist could appropriately treat it in the community by providing first aid and dressing advice,’ Dr van Tienen said.
‘The pharmacist should advise the parent to watch out for [significant] blistering, the blisters breaking, any signs of infection or excessive [levels] of pain.’
Indicators that should prompt further action include if the child:
- has a larger burn (for example, five times the child’s hand size)
- put their hand in the pot and the fingers were involved
- was splashed with hot water leading to a circumferential burn on a limb.
‘When these sorts of things occur, the patient would need to be referred,’ she said. ‘Even if the circumference of the burn wasn’t bigger than five hands, the pharmacist would still need to refer the patient on if there was swelling and the potential for complications.’
Why does timely first aid and follow-up matter?
Adequate first aid – at least 20 minutes of cool running water within 3 hours of the injury – can significantly affect the size, depth and outcome of the burn wound, Ms Schrale said.
‘Burns are very painful and can also be itchy. At times, dressings leak or slip or get wet,’ she said. ‘These issues often need to be escalated after hours when the patient’s GP or the burns outpatient clinic have limited availability. Community pharmacies also assist EDs by reducing the load and wait times for minor injuries that could be managed through primary care.’
The resources are applicable to all pharmacy staff, Dr van Tienen said.
‘It’s definitely a good resource to guide pharmacy assistants as to what is within their scope to manage and what they need to refer as well,’ she said.
The new Pharmacists Advisory Card and A3 Poster is available here. To support further training of staff, pharmacists can refer to the Burns section in the Australian Pharmaceutical Formulary and Handbook.




 Owner of Canberra's Capital Chemist Southlands Louise McLean MPS.[/caption]
Owner of Canberra's Capital Chemist Southlands Louise McLean MPS.[/caption]

 Supplied by CSL Seqirus[/caption]
Supplied by CSL Seqirus[/caption]


 Tahnee Simpson[/caption]
Tahnee Simpson[/caption]
 Nicolette Ellis MPS[/caption]
Nicolette Ellis MPS[/caption]






