Research highlights the vital role HMRs play in averting medicine misadventure.
In 2016, members of the PSA Accredited Pharmacist Leadership Group (APLG) undertook an audit to determine the clinical impact of HMRs on patients. The aim of this audit was to 1) determine the range of drug-related problems (DRPs) encountered by accredited pharmacists (APs), and 2) investigate the types of recommendations APs provided to general practitioners (GPs) in their HMR reports. Seven accredited pharmacists from the APLG practising across Australia conducted a personal clinical audit of their most recently completed HMRs.
The data of 130 patients who received the HMR service was anonymously collected. The demographics of these patients is described in Table 1. Most patients were female (61%), living in an urban area (92%), with an average age of 74.4 years. The number of medications recorded at the time of the HMR was significantly higher than the number of medications listed on the GP referral (p<0.05).
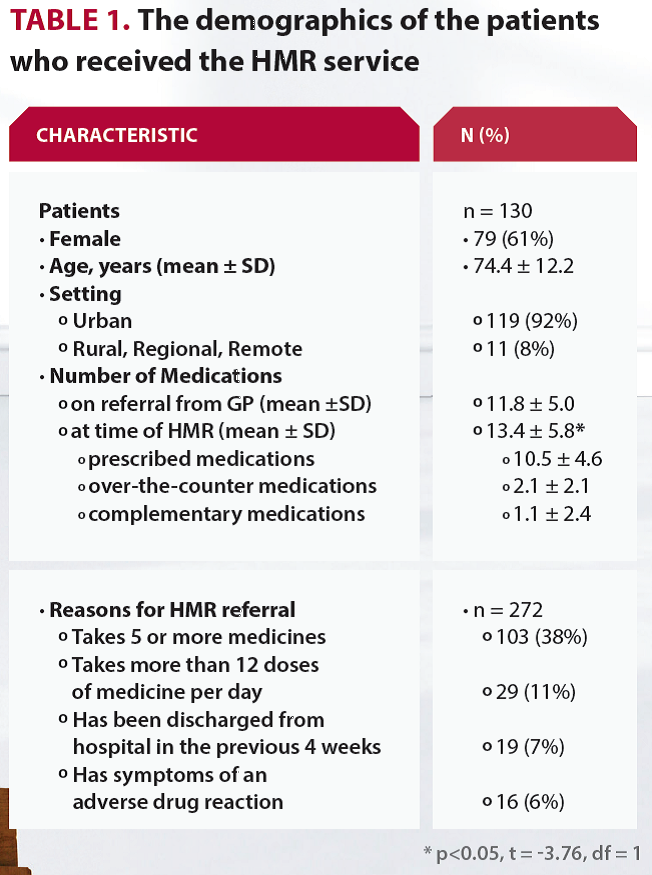
The most common DRPs were associated with drug selection (26.7%), over/under prescription (20.0%), untreated indications (13.9%) and compliance/concordance (12.0%). The top three recommendations written by APs were qualitatively analysed to determine the key words used within the recommendations (Figure 1). The key words ‘dose’, ‘reduce’, ‘cease’ and ‘change’ are predominately associated with recommendations for dose reduction and deprescribing.
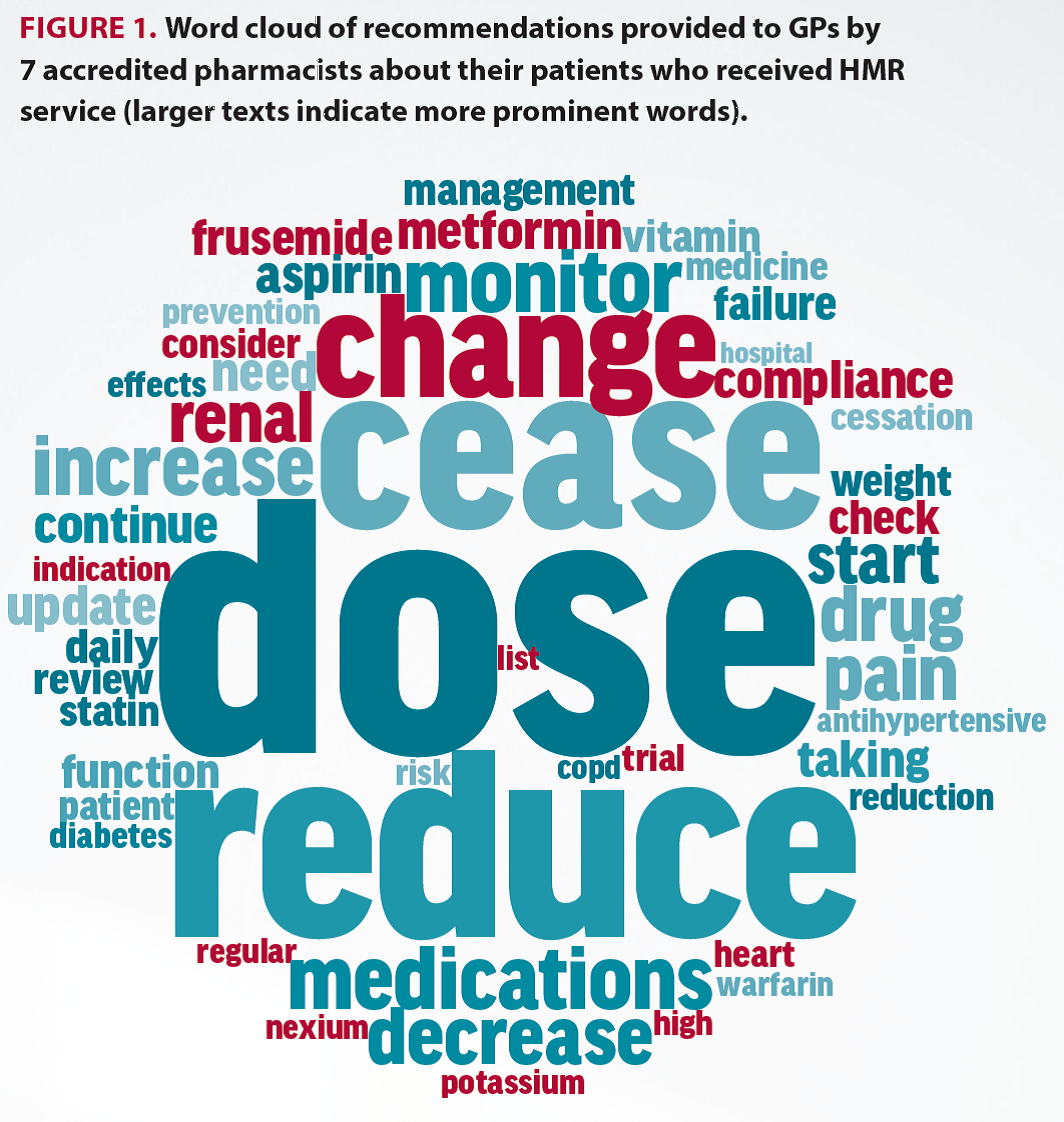
This audit has identified the extent of DRPs for patients receiving the HMR service as identified by APs. Most patients were identified as having hyperpolypharmacy (prescribed 10 or more medications), and there was a significantly higher number of medications identified during the HMR compared with the medications listed on the GP referral. The majority of DRPs were associated with drug selection, with ‘no apparent indication’ commonly identified. The main key words used within the top three recommendations were associated with dose reduction and deprescribing. This is consistent with the findings of a recent systematic review that demonstrated medication reviews are an important intervention to reduce DRPs.2
HMRs have consistently been shown to be a valuable intervention in identifying DRPs and improving clinical outcomes. A review of pharmacist-led medication review interventions supported the value of medication review for a range of clinical outcomes, such as positive impacts on glycosylated haemoglobin, blood pressure, cholesterol and medication appropriateness.3
While there will always be a level of unavoidable risk of harm associated with medication use, a substantial proportion of harms are considered to be avoidable. In a review of studies investigating the prevalence of drug-related hospital admissions in Australia, 32–69% were definitely or possibly preventable.4 HMRs (and MMRs) have an important role in identifying DRPs with the potential to reduce avoidable drug-related harm.
However, in a recent prospective cohort investigation of adults aged 45 and over in Australia, HMR was common in individuals with polypharmacy and hyperpolypharmacy, but HMR use over a 5-year period was generally below 10%, even in high-risk groups, suggesting poor uptake of the HMR service.5
Therefore, given the positive impacts of MMRs, there is a need to encourage and maximise its implementation for patients who are predisposed to medication misadventure.
Conclusion
This audit has demonstrated that HMRs are valuable in identifying a range of DRPs in patients. APs commonly recommend changes to medications that include dose reduction or deprescribing. The results of this study were provided to a submission on behalf of the APLG to the Australian Government Review of Pharmacy Remuneration and Regulation.
Further information
Read the PSA Guidelines for HMRs at: www.psa.org.au/download/practice-guidelines/home-medicines-review-services.pdf
PSA offers a preparatory stage 1 course for pharmacists wishing to undertake MMRs at: www.psa.org.au/mmr
Learn more at www.australianpharmacist.com.au
Acknowledgements
The authors would like to acknowledge the members of the 2016 Accredited Pharmacist Special Interest Group: Andrew Stafford (WA), Sue Scott (QLD), Angus Thompson (TAS), Jenny Gowan (VIC), Amy Page (VIC), Katja Naunton-Boom (ACT), and Trish Russell (ACT). Lisa Kouladjian O’Donnell would like to acknowledge the work of the previous chair of the Accredited Pharmacist Special Interest Group, Susan Edwards, for initiating this audit and her contributions to the Australian Government Review of Pharmacy Remuneration and Regulation on behalf of the group.
Current members of the APLG are: Dr Lisa Kouladjian O’Donnell (Chair), Hayley Croft (NSW), Susan Edwards (SA), Dr Jenny Gowan (VIC), Saloni Shah (WA), Sue Scott (QLD), Fran Vaughan (NT), Emmanual Pippos (QLD) and Himali Kaniyal (PSA Secretariat).
References
- Williams M. et al. Int J Clin Pharm, 2012;34:43-52. DOCUMENT: a system for classifying drug-related problems in community pharmacy. At: https://www.ncbi.nlm.nih.gov/pubmed/22101425
- Kallio SE. et al. JAGS 2018; 66(8):1613-1620. Community Pharmacists’ contribution to medication reviews for older adults: a systematic review. At: https://www.ncbi.nlm.nih.gov/pubmed/29972691
- Jokanovic N et al. RSAP 2017; 13(4):661-685. Pharmacist-led medication review in community settings: An overview of systematic reviews. At: https://www.ncbi.nlm.nih.gov/pubmed/27665364
- Pharmaceutical Society of Australia 2019. Medicine Safety: Take Care. Canberra: PSA. Available from: psa.org.au/wp-content/uploads/2019/01/PSA-Medicine-Safety-Report.pdf
- Du W. et al. BMJ Open 2019; 9(2): e027305 Patterns of high-risk prescribing and other factors in relation to receipt of a home medicines review: a prospective cohort investigation among adults aged 45 years and over in Australia. At: https://bmjopen.bmj.com/content/9/2/e027305



 John Jones MPS, pharmacist immuniser and owner of My Community Pharmacy Shortland in Newcastle, NSW[/caption]
John Jones MPS, pharmacist immuniser and owner of My Community Pharmacy Shortland in Newcastle, NSW[/caption]


 Debbie Rigby FPS explaining how to correctly use different inhaler devices[/caption]
Debbie Rigby FPS explaining how to correctly use different inhaler devices[/caption]




 Professor Sepehr Shakib[/caption]
Professor Sepehr Shakib[/caption]

 Lee McLennan MPS[/caption]
Lee McLennan MPS[/caption]
 Dr Natalie Soulsby FPS, Adv Prac Pharm[/caption]
Dr Natalie Soulsby FPS, Adv Prac Pharm[/caption]
 Joanne Gross MPS[/caption]
Joanne Gross MPS[/caption]





