The LGBTQIA+ community experiences poorer health outcomes than other Australians. As Sydney plays host to the WorldPride festival in February and March, it’s time for the entire health system – including pharmacists – to step up.
When 31-year-old trans man Sean* attempted to obtain emergency contraception from his local pharmacy, ‘it felt like everything that could go wrong, did’.
‘I’m masculine presenting, and when I explained it was for me and not a partner, the pharmacist didn’t know how to treat me,’ he says. ‘They asked a lot of personal questions about my gender identity and sexuality at the counter, where other people were waiting. I ended up leaving and asking a friend to come with me to a different pharmacy.’
Four years on, Sean says the incident has made him hesitant to access other health services for fear he will receive similar treatment. ‘I felt so unwelcome, uncomfortable and embarrassed,’ he says. ‘No one should be made to feel that way.’
Sean isn’t alone in his experience of the healthcare system as a member of the lesbian, gay, bisexual, transgender, queer, intersex, asexual and other diverse gender or orientation (LGBTQIA+) community.† Members of this community report they experience everything from uncomfortable conversations to facing unsafe environments, lack of understanding about their health needs, incorrect assumptions, and being misgendered or misnamed.
Healthcare professionals often assume the person standing in front of them is a heterosexual, cisgender person, says LGBTIQ+ Health Australia CEO Nicky Bath (she/her). ‘Often, services just aren’t well equipped to work with people who have diverse genders and sexualities, or who are intersex … But it’s critical when accessing a service that you can be your authentic self. Otherwise, you’ll always be protecting parts of yourself for fear of repercussions should you disclose them.’
A fear of discrimination when accessing health care can have a direct impact on LGBTQIA+ people’s physical and mental health. In a 2019 study, 71% of LGBTQIA+ people reported they did not seek a support service during their most recent personal or mental health crises, with ‘anticipation of discrimination’ highlighted as one of the key barriers. More than half of respondents said they relied on peers or self-coping methods instead, including self-harm or alcohol and other drugs.1
Meanwhile, a report from UK charity Stonewall found 1 in 7 ‘LGBT people’ avoided seeking health care for fear of discrimination from staff. Of those who did seek support, 1 in 8 reported experiencing some form of unequal treatment.2 And in the United States, a survey of more than 6,000 transgender people found 28% of respondents delayed seeking care to avoid discrimination.3
As Sean’s experience shows, the pharmacy profession isn’t exempt. According to the UK LGBT Foundation’s Pride in Practice Patient Experience Survey 2021, 1 in 20 people experienced some form of discrimination or unfair treatment based on their sexual orientation, gender identity or trans status from their pharmacy within the last 12 months. Additionally, 73% of trans and non-binary respondents did not share their gender identity or gender history with their pharmacist.4
‘Being able to have [personal] conversations with pharmacists from a place of safety as someone who may be ‘L’ or ‘G’ or any of the acronyms is vital,’ Ms Bath says. ‘Otherwise, particular health considerations can be missed and people will not get the best health care.’
Recognising this, PSA has recently released a Position Statement on Equality (February 2023), in which it ‘insists on equitable access to inclusive, appropriate and discrimination-free health care and strongly advocates for equality for all LGBTQIA+ [people]’.
It calls for actions such as including LGBTQIA+ health education in all Australian pharmacy programs; ensuring pronouns and chosen names can be used in healthcare systems; using inclusive language; and recognising partners or a person’s family of choice as legally authorised decision makers in relation to health care.
Health inequalities
Of course, LGBTQIA+ people aren’t a homogenous group and many lead happy, healthy lives – but health inequities do exist compared to Australians generally.
Research shows lesbian and bisexual women and gay men in Australia are twice as likely to be diagnosed with cancer compared to the heterosexual population. This may be due in part to higher rates of smoking, about double the national average, according to QUIT Victoria,6 and alcohol consumption and low rates of cancer screening in LGBTQIA+ communities.7
LGBTQIA+ people are also more likely to have depression, anxiety, be diagnosed with a mental health disorder, have suicidal ideation, have engaged in self-harm and/or have attempted suicide in their lifetime.7 The rates of domestic violence in same-sex relationships are also higher compared to heterosexual people.7
In some good news, daily smoking had decreased in people identifying as LGBTIQ from 28% in 2010 to 16% in 2019 and recent use of any illicit drug had gone from 36% to 16% over the same period.8 But in the 12 months prior to 2019, lesbian, gay or bisexual people were nine times as likely to use illicit drug inhalants as those in the general community, nearly four times as likely to use methamphetamine and amphetamines, 3.5 times as likely to use hallucinogens and twice as likely to use ecstasy.8
Health outcomes for LGBTQIA+ people can be poorer depending on where in the country they live, socioeconomic status, age, whether they identify as Aboriginal or Torres Strait Islander or if they have a disability.
As such, LGBTQIA+ people are identified as a priority population in a range of national strategies, including the National Medicines Policy,9 National Drug Strategy,10 National Alcohol Strategy,11 National Men’s Health Strategy,12 National Women’s Health Strategy13 and the National Mental Health and Suicide Prevention Plan.14 In the 2022/23 federal Budget, $1.3 million was allocated to ‘explore the unique health issues and barriers to access care faced by LGBTIQ+ Australians’.15
‘Experiences of stigma and discrimination in healthcare settings make access to appropriate care difficult,’ says Dr Natalie Amos (she/her), a Research Offer at the Australian Research Centre in Sex, Health and Society. ‘It’s also difficult to find care that is affirming of LGBTQIA+ identities and knowledgeable enough to be able to provide adequate care and meet their needs.’
Making progress
Much of the health inequity LGBTQIA+ people face is systemic and requires large-scale change to correct, such as including LGBTQIA+ people in the census, which could help shape health policy.
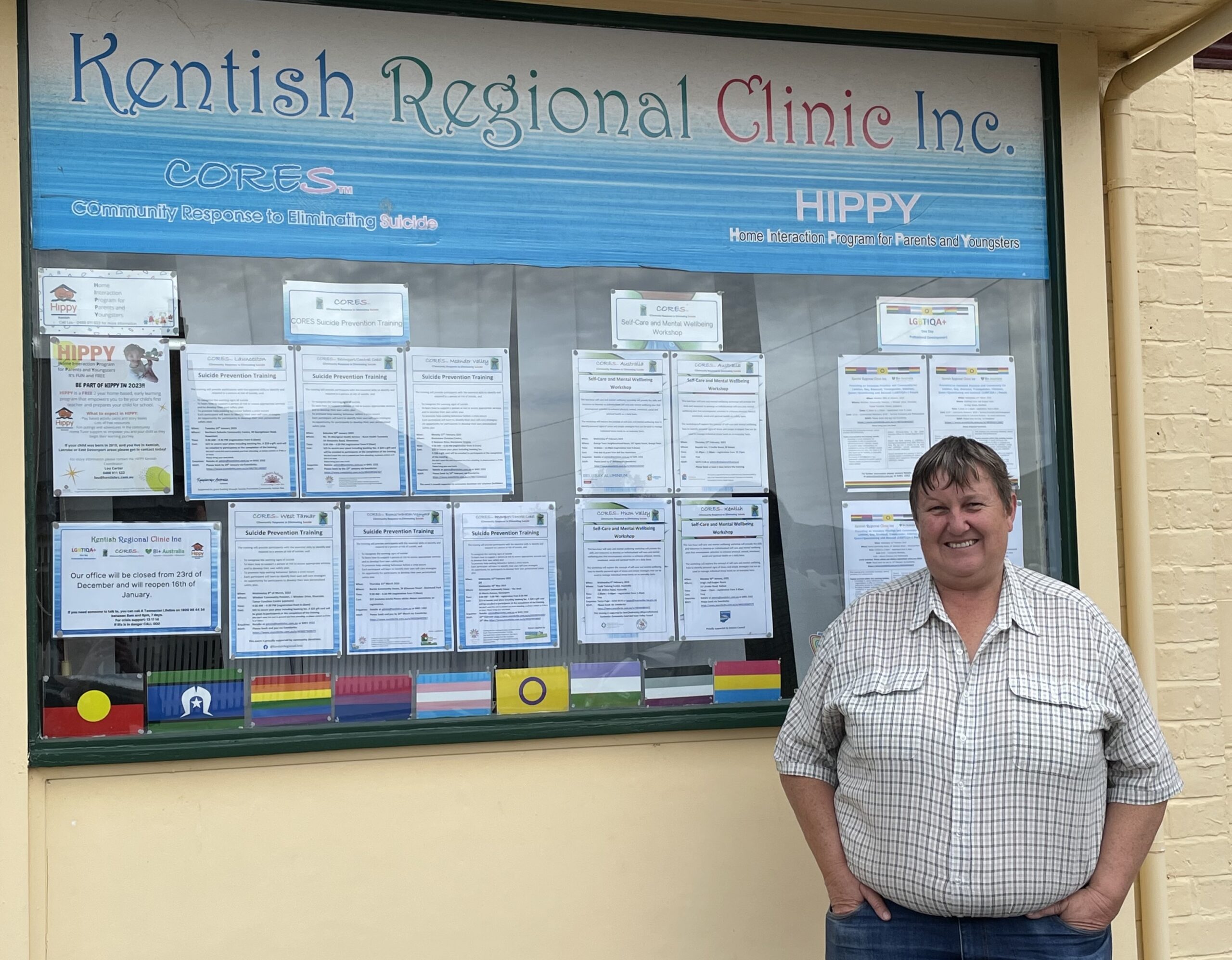
On a local scale, some employers have taken action to help ensure pharmacies are inclusive, safe environments by creating an online learning series to help team members better understand how to provide appropriate patient-centred care. Topics covered include the barriers and health disparities faced by the LGBTQIA+ community, why language matters and how pharmacists can become allies.
Brenton Hart MPS (he/him) helped to develop this training along with other TerryWhite Chemmart pharmacists, NSW health promotion organisation ACON, Pride in Health + Wellbeing and LGBTQIA+ community members.
‘We heard some truly horrifying stories of people feeling isolated, alone and unsupported across the entire healthcare system, including in pharmacy,’ Mr Hart says. ‘Creating a more inclusive environment is only a small step but one we see as vitally important’.
‘The best thing to come from our education offering is the conversations that have happened within our teams. It’s so important that these topics can be spoken about openly, in the hope that simple changes can occur in the way we interact with members of all vulnerable communities, and in the way we operate our pharmacies.’
These changes include using dispensing software to record a person’s preferred names and pronouns, as well as being aware of local LGBTQIA+ services, including support for family and loved ones.
‘We now also encourage all our team members to include their preferred pronouns on their name badge, and we are also able to display a range of flags, including the pride flag, which I have chosen to do,’ Mr Hart says. ‘It makes me proud every time I put it on.’
Becoming an ally
Brent Mackie (he/him), ACON’s Director of Policy, Strategy and Research says many pharmacists already provide a positive environment for their LGBTQIA+ patients, but more can be done.
‘We’ve had HIV medications for a long time, so pharmacists have worked through that, but areas like gender affirming care are newer … Pharmacists could facilitate workshops where community members go through what works and what doesn’t. It’s about making the consumer feel comfortable and secure in the space.’ Maintaining confidentiality is also important, with Mr Mackie encouraging pharmacists to offer to speak with patients in a separate counselling room if possible.
Other steps pharmacists can take include putting up signage that makes it clear LGBTQIA+ people are welcome, and signposting specific services, such as the availability of PrEP and PEP. Hospital pharmacists, for instance, could wear a badge with pronouns/flags and their organisation or business, if permitted. Businesses can also opt to become a ‘safe place’ and display a rainbow sticker in their window through programs such as ACON’s Welcome Here initiative.
However, Ms Bath warns this must go beyond window dressing. ‘If we come in thinking we’re welcome, then there’s a need for all the staff in the pharmacy to be signed up to deliver a service that reinforces that,’ she says.
Ultimately, her advice is simple: ‘Be open to the person in front of you, be curious about their story, don’t make assumptions and be really kind.’
References
- Waling A, Lim G, Dhalla S, Lyons A, et al. Understanding LGBTI+ lives in crisis. Australian Research Centre in Sex, Health and Society, La Trobe University and Lifeline Australia. 2019.
- Bachmann CL, Gooch B. LGBT in Britain: health report. Stonewall. 2018. At: www.stonewall.org.uk/system/files/lgbt_in_britain_health.pdf
- Grant JM, Mottet LA, Tanis J. Injustice at every turn: a report of the national transgender discrimination survey. National Center for Transgender Equality and National Gay and Lesbian Task Force. 2011. At: https://transequality.org/sites/default/files/docs/resources/NTDS_Report.pdf
- Pride in practice LGBT patient experience survey 2021. LGBT Foundation. 2022. At: https://lgbt.foundation/news/pride-in-practice-lgbt-patient-experience-survey-2021/476
- Bourne A, Carman M, Hill AO, et al. Australian Research Centre in Sex, Health and Society, la Trobe University. Private lives 3: the health and wellbeing of LGBTIQ people in Australia. 2020. At: https://bit.ly/3HsztY9
- QUIT Victoria. Helping people in LGBTIQ+ communities to quit. 2023. At: www.quit.org.au/articles/lgbtiq/
- Australian Government Department of Health. National Preventive Health Strategy 2021–2030. 2021. At: www.health.gov.au/sites/default/files/documents/2021/12/national-preventive-health-strategy-2021-2030_1.pdf
- Australian Institute of Health and Welfare. Factsheet – People identifying as lesbian, gay, bisexual, transgender, intersex or queer. 2022. At: https://www.aihw.gov.au/getmedia/16be9d5c-7bf5-4700-ba84-8c2174804f5d/PHE-221-Factsheets-LGBTIQ.pdf.aspx
- Australian Government Department of Health and Aged Care. National Medicines Policy 2022. At: www.health.gov.au/sites/default/files/2022-12/national-medicines-policy.pdf
- Australian Government Department of Health. National Drug Strategy 2017–2026. 2017. At: www.health.gov.au/sites/default/files/national-drug-strategy-2017-2026.pdf
- Australian Government Department of Health. National Alcohol Strategy 2019–2028. 2019. At: www.health.gov.au/sites/default/files/documents/2020/11/national-alcohol-strategy-2019-2028.pdf
- Australian Government Department of Health. National Men’s Health Strategy 2020–2030. 2019. At: www.health.gov.au/sites/default/files/documents/2021/05/national-men-s-health-strategy-2020-2030.pdf
- Australian Government Department of Health. National Women’s Health Strategy 2020–2030. 2018. At: www.health.gov.au/sites/default/files/documents/2021/05/national-women-s-health-strategy-2020-2030.pdf
- Australian Government Department of Health. National Mental Health and Suicide Prevention Plan. 2021. At: www.health.gov.au/sites/default/files/documents/2021/05/the-australian-government-s-national-mental-health-and-suicide-prevention-plan-national-mental-health-and-suicide-prevention-plan.pdf
- Butler M. Budget October 2022–23: Strengthening Medicare. Department of Health and Aged Care. 2022. At: www.health.gov.au/ministers/the-hon-mark-butler-mp/media/budget-october-2022-23-strengthening-medicare
- Australian Human Rights Commission. Face the facts: lesbian, gay, bisexual, trans and intersex people. 2014. At: https://humanrights.gov.au/sites/default/files/7_FTF_2014_LGBTI.pdf
- LGBTIQA+ Health Australia. Snapshot of Mental Health and Suicide Prevention Statistics for LGBTIQ+ People. 2021. At: www.lgbtiqhealth.org.au/statistics
- Morandini JS, Blaszczynski A, Dar-Nimrod I, et al. Minority stress and community connectedness among gay, lesbian and bisexual Australians: a comparison of rural and metropolitan localities. Aust NZ J Public Health 2015;39:260–6.
- Langdon E, Kavanagh P, Bushell M. Exploring pharmacists’ understanding and experience of providing LGBTI healthcare. Explor Res Clin Soc Pharm 2022;6. Epub 2022 April 9.



 Kelly Abbott MPS[/caption]
Kelly Abbott MPS[/caption]


 Owner of Canberra's Capital Chemist Southlands Louise McLean MPS.[/caption]
Owner of Canberra's Capital Chemist Southlands Louise McLean MPS.[/caption]

 Supplied by CSL Seqirus[/caption]
Supplied by CSL Seqirus[/caption]