td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31034
[post_author] => 3410
[post_date] => 2025-12-08 14:06:18
[post_date_gmt] => 2025-12-08 03:06:18
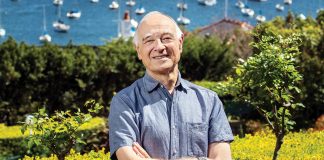
[post_content] => Professor Mark Naunton MPS, Chair of the Faculty of Health and Professor of Pharmacy at the University of Canberra, was unanimously elected by the PSA Board to serve as the next president from January 2026.
The Board has also elected Bridget Totterman MPS as National Vice President (elect) to fill the vacancy created by Prof Naunton’s election.
[caption id="attachment_31037" align="aligncenter" width="600"] Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
What motivated you to seek election as the next PSA National President?
I’ve had a long career in pharmacy, working across academia, research and education – but like most pharmacists, I started in community pharmacy.
As an intern, my preceptor was a PSA branch committee member and he paid for my PSA membership. From the very beginning, it was instilled in me how important it is to give back to the profession.
In research, I saw firsthand the gaps in our healthcare system, which drove me to explore how pharmacists can help to improve care – particularly in transitions of care. I’ve also worked in educational outreach with GPs and pharmacists, showing me how much GPs actually value pharmacists; when we communicate well and have something reasonable to say, they listen. That has always been my experience as a forward-facing clinical pharmacist
My shift into academia was driven by wanting to train the next generation of pharmacists. What I often saw in students wasn’t a lack of knowledge, but a lack of confidence – something I’m keen to address.
A consistent theme throughout my career has been the dedication of pharmacists – and how much more we could achieve with recognition, support and the right structures in place.
I’ve always wanted to use my voice to ensure our profession is heard at the highest level. I believe PSA must continue to lead with strength, vision and, above all, unity – so that our profession can not only cope with change, but thrive through it.
What do you hope to achieve as PSA President?
Recognition and remuneration that truly reflects our expertise as medicines experts are big priorities. We have a highly predominantly female workforce, including PSA’s board. There are pay inequities affecting female pharmacists that must be addressed.
I also want to strengthen PSA’s role as the national leader in pharmacy advocacy. Under Associate Professor Fei Sim’s tenure, PSA has grown significantly in this space, and I want to build on that legacy by ensuring every pharmacist feels supported, valued and confident in their practice.
That includes pharmacists across all settings – from community to hospital, general practice, aged care, academia, industry and government. We need to support and recognise the whole profession.
Fei has been a truly inspirational leader, overseeing the negotiation of the first Strategic Agreement of Pharmacist Professional Practice, establishing the PSA Foundation, driving the strategic agenda for innovation in quality use of medicines, and driving practice forward through her membership of numerous government advisory committees.
[caption id="attachment_31039" align="aligncenter" width="600"] A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
Why do you feel this is such a pivotal moment for PSA and the profession?
The PSA is undergoing a major acquisition of the Australasian College of Pharmacy. Our members voted for it because they believe it’s in the best interests of PSA and the profession, helping us strengthen advocacy, improve our education platform, expand resources, and grow our membership.
Through the acquisition, we also want education and member benefits to become more affordable for pharmacists. Cost-of-living pressures are very real, and we need members to feel that PSA genuinely has their back, making their job easier so they can practise to full scope.
At the same time, healthcare is evolving rapidly. Patients need more accessible and innovative care, with pharmacists uniquely positioned to meet those needs.
Primary care reform is happening now – and this is the moment for PSA to champion pharmacists and ensure we’re at the centre of tomorrow’s healthcare system.
What are the major challenges pharmacists are facing right now?
Workforce sustainability is, and will continue to be a significant issue now and into the near future.
While recognition of our clinical expertise is improving, especially with expanded scope of practice and pharmacist prescribing, it's still new – with awareness and acceptance being ongoing challenges.
COVID-19 highlighted what pharmacists can do exceptionally well, particularly vaccinations.
But pharmacists are stretched, with many competing demands taking a toll. Ensuring pharmacists are properly remunerated and supported is critical to maintaining the sustainability of the profession. My role is to ensure they have a voice at every level.
How do you see the profession evolving in 5 years?
Five years ago, we were doing little more than flu vaccinations. Now we’re administering a much broader range of vaccines nationally. Governments are increasingly looking for more efficient healthcare delivery, and pharmacists have shown we can answer that call. But to continue along this path, we need better-trained pharmacy assistants, because pharmacists can’t do more unless we hand over some tasks.
Another area where we still need to make headway is medicine safety. Pharmacists are trained to ensure patients get the right medicine at the right time, and we have highly skilled pharmacists providing medicines reviews – yet many are constrained by caps and limits that make no sense clinically.
In 5 years’ time, I want to see those barriers gone, so patients can actually receive the expertise pharmacists are ready and willing to provide.
I also want to see pharmacists better integrated into healthcare teams, both physically and digitally. That might mean pharmacists embedded in general practice, or pharmacists who are digitally connected to practices and other care settings. We’re a large country and we know there is a shortage of pharmacists – so we have to find creative ways to connect our expertise to where it’s needed.
How have your background and previous experiences shaped your views of the profession?
I grew up in rural Tasmania and have done a lot of work across rural and regional Australia. I know those communities don’t always feel supported. I understand the challenges facing patients, healthcare workers and pharmacists in those areas, and I want them to know that I hear them.
I’d like people in rural and regional communities to feel they can pick up the phone and talk to me – and to see me as someone who genuinely has their back, just as much as pharmacists in our cities.
I’ve also lived and worked in the Netherlands, where they have often been at the forefront of innovation in data and system design. They have shown what’s possible when you really line up systems to support better care.
I’d like to draw on those experiences and share them with the right people here, because I believe we can learn a great deal from our overseas counterparts as we strengthen pharmacy practice and medicine safety in Australia.
[post_title] => PSA’s new president wants to transform the profession
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => psas-new-president-wants-to-transform-the-profession
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-08 15:16:16
[post_modified_gmt] => 2025-12-08 04:16:16
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31034
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => PSA’s new president wants to transform the profession
[title] => PSA’s new president wants to transform the profession
[href] => https://www.australianpharmacist.com.au/psas-new-president-wants-to-transform-the-profession/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31035
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31020
[post_author] => 3410
[post_date] => 2025-12-03 11:10:54
[post_date_gmt] => 2025-12-03 00:10:54
[post_content] => These case examples show that errors arise from system pressures, not individual failings. Pharmacists can act on these insights to strengthen governance.
When pharmacists call Pharmaceutical Defence Limited (PDL), they’re often navigating some of the most stressful moments of their professional lives.
Behind the scenes, PDL’s professional officers, including pharmacist Claire Bekema – who is also a professional practice pharmacist at PSA – talk pharmacists through clinical decisions, regulatory notifications and incident management.
Here, Ms Bekema outlines the top incidents reported to PDL, alongside practical strategies to reduce risk and respond safely when something goes wrong.
Wrong-patient supply leads to hospital admission
Wrong-patient incidents remain one of the most common and serious error types, often occurring when workflow pressures and assumptions collide.
‘That might be when you call out a script for “[one surname], and somebody just turns up and says, “Yep, that’s me,” and they take it out the door,’ Ms Bekema told participants of PSA’s Voices of Pharmacy – Passion, Purpose, and Possibility webinar last week (26 November).
In one case, which occurred after 60 Day Dispensing was implemented, a patient received two boxes of multiple medicines that were not theirs.
‘It was high-dose antihypertensives, and the patient had low health literacy, so they didn’t know what they were expecting to receive from the doctor,’ she said.
‘They picked up this other person’s medicines and they took one from each box. So they took really high doses of antihypertensives all at once.’
Once errors such as this are discovered, Ms Bekema is clear about what the next steps should be.
‘In this particular scenario, I said, “Let’s talk about the incident and how it occurred later, but the first thing is: try and track down this patient and make sure they’re receiving medical attention”,’ she said.
‘They ended up being transferred to hospital by ambulance because their blood pressure was [extremely low]. Wrong-patient errors can have pretty dire consequences.’
For more information, refer to previous AP coverage on:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31014
[post_author] => 9164
[post_date] => 2025-12-01 15:34:25
[post_date_gmt] => 2025-12-01 04:34:25
[post_content] => The Therapeutic Goods Administration (TGA) has today (Monday 1 December) made updates to product warnings for GLP-1 and dual GIP/GLP-1 receptor agonists for two separate safety issues.
AP examines what pharmacists need to know.
ALERT 1: Potential risk of suicidal thoughts
The TGA has aligned product warnings for all GLP-1 RA medicines to ensure consistent information regarding the potential risk of suicidal thoughts or behaviours.
There have been growing questions about whether there’s a link between GLP-1 RAs and suicidal ideation. As of 23 September 2025, the TGA’s Database of Adverse Event Notifications (DAEN) contains the following:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31010
[post_author] => 3410
[post_date] => 2025-12-01 11:52:12
[post_date_gmt] => 2025-12-01 00:52:12
[post_content] => Australia’s east coast was belted with heavy storms last week. Spring and summer storms can trigger thunderstorm asthma – with bursts of pollen often causing sudden, severe asthma attacks, particularly in patients with asthma or allergic rhinitis.
‘There was the big event in Victoria in November 2016 when 10 people died,’ said Clinical Associate Professor Debbie Rigby FPS, pharmacist and Clinical Executive Lead, National Asthma Council Australia (NAC).
‘But there are other peaks that don’t get as much media coverage – for example, there was terrible weather on Melbourne Cup Day this year, and data showed there were over 100 emergency department (ED) admissions and ambulance callouts that day.’
When asthma symptoms spike, so do SABA (short-acting beta2-agonist) requests. With new guidelines that discourage overreliance on SABA, asthma expert A/Prof Rigby explains how pharmacists should manage these situations.
What do the new asthma guidelines say?
In the updated NAC Australian Asthma Handbook, released in September 2025, a key guideline change is that no adult or adolescent with asthma should be using salbutamol alone.
‘Every [adult or adolescent] with confirmed asthma now needs to be on an inhaled corticosteroid (ICS),’ A/Prof Rigby said.
The National Asthma Council recently released data that found there were 478 asthma-related deaths in 2024, equating to more than one per day.
There was a surprising increase in asthma deaths in the youngest patient cohort, those aged 0 to 35.
‘This is largely due to poorly controlled asthma, including people over-relying on SABA, not using preventers, or not using anti-inflammatory reliever therapy,’ Ms Rigby said. ‘Those with more severe symptoms should be on maintenance-and-reliever therapy, or MART.’
But that doesn't mean pharmacists should deny patients salbutamol, particularly during events such as storms that can trigger exacerbations.
‘Absolutely supply it if a patient has symptoms – it’s potentially life-saving during an acute episode – but we should be alluding to the fact that it’s risky to use salbutamol alone in asthma,’ she said. ‘‘Use it as an opportunity to explain that the guidelines have changed and that we now have better treatment, but also assess them to determine if they need to see a GP straightaway or go to ED.’
For example, if a patient can’t finish a sentence without taking a breath, they need immediate treatment.
Pharmacists should also remind patients that they should have an asthma action plan, which many adults don’t have. ‘Most people can manage with salbutamol in an acute situation – but they can also use budesonide-formoterol.’
It’s also important to point out the benefits of preventative and anti-inflammatory therapy, including improved asthma control and long-term health outcomes.
‘ICS–formoterol reduces the risk of severe episodes, it's more convenient because you only carry one inhaler and even has environmental benefits,’ A/Prof Rigby said. ‘There are about 15 million salbutamol inhalers used annually, which is a significant carbon footprint.’
What can pharmacists do?
A lot has been learned since the 2016 thunderstorm asthma event, A/Prof Rigby said.
‘The Victoria Department of Health has been very proactive with the pollen-alert apps that give daily high-pollen warnings,’ she said.
There are also similar systems in other states; these apps provide a daily alert using a traffic-light system across mapped regions.
‘For example [on Thursday], the Mildura area was “red” – very high pollen count,’ A/Prof Rigby said.
‘I encourage all pharmacists to sign up, but also to recommend them to patients with asthma and/or allergic rhinitis. When your area is on medium or high alert, pharmacists should be having conversations with patients about being prepared.’
This includes always having a reliever on hand – either salbutamol, or preferably, the anti-inflammatory reliever budesonide-formoterol.
‘During thunderstorm asthma – the “perfect storm” of high pollen plus thunderstorms – people should also avoid being outside, close windows, use air-conditioning, and in cars set air recirculation mode,’ she said.
And when patients present to the pharmacy for treatment for allergic rhinitis, pharmacists should ask: Do you have asthma?
‘Around 80% of people with asthma also have allergic rhinitis, and 40–60% of people with allergic rhinitis also have asthma,’ A/Prof Rigby said. ‘We need to think about “one airway, one disease.” If you get the nose under control, you get better asthma control – and vice versa.’
What’s the approach when it’s not asthma?
During the 2016 thunderstorm asthma event, many people who presented to pharmacies or EDs didn’t have diagnosed asthma, A/Prof Rigby said.
‘Many had hay fever or allergic rhinitis,’ she said. ‘So when people request hay fever treatments, pharmacists should ask about symptoms – such as shortness of breath, cough or chest tightness – which could indicate asthma.’
When these incidents occur, pharmacists should ask whether patients had childhood asthma, hay fever or other respiratory issues. They can also provide Asthma first aid.
‘You can supply a salbutamol puffer – ideally with a spacer – because when people are short of breath they’re less able to coordinate inhalation, and most people don’t use puffers correctly anyway,’ she said.
Pharmacists should use the 4x4x4 method: 4 puffs, one at a time, via a spacer; wait 4 minutes; repeat as needed.
‘If the patient is still short of breath, seek medical advice,’ A/Prof Rigby added. ‘And document everything.’
Pharmacists should also follow-up via phone, text or the next visit.
How should COPD be managed in a storm?
While asthma is reversible with good control, chronic obstructive pulmonary disease (COPD) involves persistent airway inflammation and irreversible obstruction.
Salbutamol may be used to relieve symptoms in patients with COPD, but it does not provide the same level of relief as it does in asthma, A/Prof Rigby said.
‘The perceived benefit of SABA for patients with COPD is often due to the person stopping and resting, or the anxiety relief of “doing something” – rather than actual bronchodilation,’ she said.
But patients with COPD are less likely to have their symptoms triggered by storms.
‘They may be short of breath at rest and have reduced exercise tolerance, so they must take preventative therapy regularly,’ A/Prof Rigby said.
This includes regular use of a long-acting muscarinic antagonist and long-acting beta2-agonist.
‘Only some patients need triple therapy,’ she added.
[post_title] => Severe spring storms show the risks of SABA overuse
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => severe-spring-storms-show-the-risks-of-saba-overuse
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-01 17:45:42
[post_modified_gmt] => 2025-12-01 06:45:42
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31010
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Severe spring storms show the risks of SABA overuse
[title] => Severe spring storms show the risks of SABA overuse
[href] => https://www.australianpharmacist.com.au/severe-spring-storms-show-the-risks-of-saba-overuse/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31013
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31004
[post_author] => 3410
[post_date] => 2025-12-01 11:40:10
[post_date_gmt] => 2025-12-01 00:40:10
[post_content] => Renal expert Carla Scuderi explains the lifelong care journey pharmacists provide to kidney disease patients.
Why specialise in kidney care?
I think kidney health chose me! I was hoping to specialise in a clinical area when a job in the Kidney Health Service came up at the Royal Brisbane and Women’s Hospital. I didn’t know what I was getting myself into, but I couldn’t believe my luck. Here was an area of specialised care in an acute hospital setting with all the feels of community pharmacy. Working in kidney health means providing cradle-to-grave care. You build long-term relationships with patients and support them through key life stages – from family planning to kidney failure and palliative care. Much of the work involves ambulatory care – comprising outpatient clinics, acute or satellite hospital dialysis settings, or home-based therapy – as well as acute inpatient admissions.
What does a kidney specialist do?
Provide medicines advice to patients and the entire multidisciplinary team and ensure medicines are available in each off-site dialysis area while coordinating the pharmacy team across these areas. This might be a visit to a dialysis unit to review new patients or a one-on-one patient consult in the clinic, followed by a consultation with the multidisciplinary team about medicine-related issues. It could also cover admissions in the emergency department through to ward rounds and reviews. Medicines access, tolerability, affordability and polypharmacy are big issues for patients with kidney disease. We also work closely with dietitians, social workers, nurses and nurse practitioners, and nephrologists.
How can community pharmacists help to identify CKD?
Over 2 million Australians are living with kidney disease and fewer than 10% of patients with chronic kidney disease (CKD) are aware they have it. Kidney Health Australia has a great handbook outlining the management of CKD in primary care, with community pharmacists being hugely important in encouraging people to get tested and supporting the lifestyle changes required to reduce the progression of CKD, such as smoking cessation.
Pharmacists can also ask patients when they last had their kidneys checked; particularly anyone with high blood pressure or diabetes. For example, if you offer blood pressure monitoring and the reading is high, ask about the kidneys. Some community pharmacies even have access to point-of-care kidney function estimation devices – brilliant!
What’s the future role of pharmacists in kidney care?
It’s an exciting time to be working in kidney care. New drugs such as sodium-glucose co-transporter 2 inhibitors, glucagon-like peptide-1 receptor agonists and non-steroidal mineralocorticoid receptor antagonists are emerging as superstars in slowing the progression of CKD. I think the future will be much more closely linked with cardiology and metabolic health rather than exclusively kidneys. The link between cardiac disease and kidney health has been given the name cardiovascular-kidney-metabolic (CKM) syndrome. Increasingly, we are using the same drugs to treat all three conditions. I also think pharmacogenomics will play a role in determining which patients are not suited to certain blood pressure medicines, for example, which will help to improve patient outcomes. Hopefully, the future will bring less reliance on dialysis, earlier diagnosis and more successful transplants – allowing people to live well and slowing the progression of CKD.
Any advice for pharmacists keen on specialising in kidney care?
Look for opportunities in adjacent fields such as cardiology and general medicine to build your knowledge. Clinical review skills, ability to perform home medicines reviews and good general drug knowledge are all essentials. You should also prepare to be confronted with blood; watching patients being put onto the dialysis machines can be confronting, particularly if you are queasy. And develop great people skills, because you’ll be with these patients for the long haul. But give it a go, it’s fantastic.
A Day in the life of Carla Scuderi, Assistant Director of Pharmacy Clinical, Royal Brisbane and Women’s Hospital, Brisbane, QLD
| 7.30 am | Early start First job of the day is to coordinate the team and manage any staffing shortfalls. Attend the hospital executive huddle to get an idea of what the day looks like, including planned admissions, surgery and discharges. |
| 8.30 am | Outpatient clinic Transplant clinic is my go-to as these patients have very complex immunosuppressant regimens and medication adherence is paramount. Ensuring we have the drug levels right and making sure patients are managing their other comorbidities, such as hypertension and diabetes, is critical. I review their pathology, weight, blood pressure, dispensing history, self-reported adherence and adverse effects – providing an updated medication list to assist with dose administration aid packing. |
| 11.00 am | Morbidity and mortality meeting Monthly all service line review of patient deaths and unexpected outcomes. This is an opportunity to review patient care, ensure systems are working appropriately and apply learnings to improve outcomes. From a pharmacy perspective, this can include ensuring access to medicines was timely. |
| 1.00 pm | Lunchtime grand rounds Lunchtimes are spent learning with the team. One of the best parts of being part of a big institution is hearing what all the other parts of the hospital do. This week grand rounds were presented by the endocrinology department, who outlined a trial on thyroid replacement treatments. |
| 2.00 pm | Statewide Renal Network meeting Weekly catch up with the Statewide coordinator and my co-chair, a nephrologist in Cairns. There’s an issue regarding potential out-of-stock supplies of a component required for dialysis. Fortunately, we discover that there isn’t a stock shortage, merely a distribution issue. |
| 4.30 pm | Home duties begin Serve as an Uber driver for the teens’ various sport, social or work commitments and ensure the home crew are fed. If I’m lucky, I can sneak in a walk around the Brisbane River or even some laps at the pool. |
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31034
[post_author] => 3410
[post_date] => 2025-12-08 14:06:18
[post_date_gmt] => 2025-12-08 03:06:18
[post_content] => Professor Mark Naunton MPS, Chair of the Faculty of Health and Professor of Pharmacy at the University of Canberra, was unanimously elected by the PSA Board to serve as the next president from January 2026.
The Board has also elected Bridget Totterman MPS as National Vice President (elect) to fill the vacancy created by Prof Naunton’s election.
[caption id="attachment_31037" align="aligncenter" width="600"] Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
What motivated you to seek election as the next PSA National President?
I’ve had a long career in pharmacy, working across academia, research and education – but like most pharmacists, I started in community pharmacy.
As an intern, my preceptor was a PSA branch committee member and he paid for my PSA membership. From the very beginning, it was instilled in me how important it is to give back to the profession.
In research, I saw firsthand the gaps in our healthcare system, which drove me to explore how pharmacists can help to improve care – particularly in transitions of care. I’ve also worked in educational outreach with GPs and pharmacists, showing me how much GPs actually value pharmacists; when we communicate well and have something reasonable to say, they listen. That has always been my experience as a forward-facing clinical pharmacist
My shift into academia was driven by wanting to train the next generation of pharmacists. What I often saw in students wasn’t a lack of knowledge, but a lack of confidence – something I’m keen to address.
A consistent theme throughout my career has been the dedication of pharmacists – and how much more we could achieve with recognition, support and the right structures in place.
I’ve always wanted to use my voice to ensure our profession is heard at the highest level. I believe PSA must continue to lead with strength, vision and, above all, unity – so that our profession can not only cope with change, but thrive through it.
What do you hope to achieve as PSA President?
Recognition and remuneration that truly reflects our expertise as medicines experts are big priorities. We have a highly predominantly female workforce, including PSA’s board. There are pay inequities affecting female pharmacists that must be addressed.
I also want to strengthen PSA’s role as the national leader in pharmacy advocacy. Under Associate Professor Fei Sim’s tenure, PSA has grown significantly in this space, and I want to build on that legacy by ensuring every pharmacist feels supported, valued and confident in their practice.
That includes pharmacists across all settings – from community to hospital, general practice, aged care, academia, industry and government. We need to support and recognise the whole profession.
Fei has been a truly inspirational leader, overseeing the negotiation of the first Strategic Agreement of Pharmacist Professional Practice, establishing the PSA Foundation, driving the strategic agenda for innovation in quality use of medicines, and driving practice forward through her membership of numerous government advisory committees.
[caption id="attachment_31039" align="aligncenter" width="600"] A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
Why do you feel this is such a pivotal moment for PSA and the profession?
The PSA is undergoing a major acquisition of the Australasian College of Pharmacy. Our members voted for it because they believe it’s in the best interests of PSA and the profession, helping us strengthen advocacy, improve our education platform, expand resources, and grow our membership.
Through the acquisition, we also want education and member benefits to become more affordable for pharmacists. Cost-of-living pressures are very real, and we need members to feel that PSA genuinely has their back, making their job easier so they can practise to full scope.
At the same time, healthcare is evolving rapidly. Patients need more accessible and innovative care, with pharmacists uniquely positioned to meet those needs.
Primary care reform is happening now – and this is the moment for PSA to champion pharmacists and ensure we’re at the centre of tomorrow’s healthcare system.
What are the major challenges pharmacists are facing right now?
Workforce sustainability is, and will continue to be a significant issue now and into the near future.
While recognition of our clinical expertise is improving, especially with expanded scope of practice and pharmacist prescribing, it's still new – with awareness and acceptance being ongoing challenges.
COVID-19 highlighted what pharmacists can do exceptionally well, particularly vaccinations.
But pharmacists are stretched, with many competing demands taking a toll. Ensuring pharmacists are properly remunerated and supported is critical to maintaining the sustainability of the profession. My role is to ensure they have a voice at every level.
How do you see the profession evolving in 5 years?
Five years ago, we were doing little more than flu vaccinations. Now we’re administering a much broader range of vaccines nationally. Governments are increasingly looking for more efficient healthcare delivery, and pharmacists have shown we can answer that call. But to continue along this path, we need better-trained pharmacy assistants, because pharmacists can’t do more unless we hand over some tasks.
Another area where we still need to make headway is medicine safety. Pharmacists are trained to ensure patients get the right medicine at the right time, and we have highly skilled pharmacists providing medicines reviews – yet many are constrained by caps and limits that make no sense clinically.
In 5 years’ time, I want to see those barriers gone, so patients can actually receive the expertise pharmacists are ready and willing to provide.
I also want to see pharmacists better integrated into healthcare teams, both physically and digitally. That might mean pharmacists embedded in general practice, or pharmacists who are digitally connected to practices and other care settings. We’re a large country and we know there is a shortage of pharmacists – so we have to find creative ways to connect our expertise to where it’s needed.
How have your background and previous experiences shaped your views of the profession?
I grew up in rural Tasmania and have done a lot of work across rural and regional Australia. I know those communities don’t always feel supported. I understand the challenges facing patients, healthcare workers and pharmacists in those areas, and I want them to know that I hear them.
I’d like people in rural and regional communities to feel they can pick up the phone and talk to me – and to see me as someone who genuinely has their back, just as much as pharmacists in our cities.
I’ve also lived and worked in the Netherlands, where they have often been at the forefront of innovation in data and system design. They have shown what’s possible when you really line up systems to support better care.
I’d like to draw on those experiences and share them with the right people here, because I believe we can learn a great deal from our overseas counterparts as we strengthen pharmacy practice and medicine safety in Australia.
[post_title] => PSA’s new president wants to transform the profession
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => psas-new-president-wants-to-transform-the-profession
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-08 15:16:16
[post_modified_gmt] => 2025-12-08 04:16:16
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31034
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => PSA’s new president wants to transform the profession
[title] => PSA’s new president wants to transform the profession
[href] => https://www.australianpharmacist.com.au/psas-new-president-wants-to-transform-the-profession/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31035
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31020
[post_author] => 3410
[post_date] => 2025-12-03 11:10:54
[post_date_gmt] => 2025-12-03 00:10:54
[post_content] => These case examples show that errors arise from system pressures, not individual failings. Pharmacists can act on these insights to strengthen governance.
When pharmacists call Pharmaceutical Defence Limited (PDL), they’re often navigating some of the most stressful moments of their professional lives.
Behind the scenes, PDL’s professional officers, including pharmacist Claire Bekema – who is also a professional practice pharmacist at PSA – talk pharmacists through clinical decisions, regulatory notifications and incident management.
Here, Ms Bekema outlines the top incidents reported to PDL, alongside practical strategies to reduce risk and respond safely when something goes wrong.
Wrong-patient supply leads to hospital admission
Wrong-patient incidents remain one of the most common and serious error types, often occurring when workflow pressures and assumptions collide.
‘That might be when you call out a script for “[one surname], and somebody just turns up and says, “Yep, that’s me,” and they take it out the door,’ Ms Bekema told participants of PSA’s Voices of Pharmacy – Passion, Purpose, and Possibility webinar last week (26 November).
In one case, which occurred after 60 Day Dispensing was implemented, a patient received two boxes of multiple medicines that were not theirs.
‘It was high-dose antihypertensives, and the patient had low health literacy, so they didn’t know what they were expecting to receive from the doctor,’ she said.
‘They picked up this other person’s medicines and they took one from each box. So they took really high doses of antihypertensives all at once.’
Once errors such as this are discovered, Ms Bekema is clear about what the next steps should be.
‘In this particular scenario, I said, “Let’s talk about the incident and how it occurred later, but the first thing is: try and track down this patient and make sure they’re receiving medical attention”,’ she said.
‘They ended up being transferred to hospital by ambulance because their blood pressure was [extremely low]. Wrong-patient errors can have pretty dire consequences.’
For more information, refer to previous AP coverage on:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31014
[post_author] => 9164
[post_date] => 2025-12-01 15:34:25
[post_date_gmt] => 2025-12-01 04:34:25
[post_content] => The Therapeutic Goods Administration (TGA) has today (Monday 1 December) made updates to product warnings for GLP-1 and dual GIP/GLP-1 receptor agonists for two separate safety issues.
AP examines what pharmacists need to know.
ALERT 1: Potential risk of suicidal thoughts
The TGA has aligned product warnings for all GLP-1 RA medicines to ensure consistent information regarding the potential risk of suicidal thoughts or behaviours.
There have been growing questions about whether there’s a link between GLP-1 RAs and suicidal ideation. As of 23 September 2025, the TGA’s Database of Adverse Event Notifications (DAEN) contains the following:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31010
[post_author] => 3410
[post_date] => 2025-12-01 11:52:12
[post_date_gmt] => 2025-12-01 00:52:12
[post_content] => Australia’s east coast was belted with heavy storms last week. Spring and summer storms can trigger thunderstorm asthma – with bursts of pollen often causing sudden, severe asthma attacks, particularly in patients with asthma or allergic rhinitis.
‘There was the big event in Victoria in November 2016 when 10 people died,’ said Clinical Associate Professor Debbie Rigby FPS, pharmacist and Clinical Executive Lead, National Asthma Council Australia (NAC).
‘But there are other peaks that don’t get as much media coverage – for example, there was terrible weather on Melbourne Cup Day this year, and data showed there were over 100 emergency department (ED) admissions and ambulance callouts that day.’
When asthma symptoms spike, so do SABA (short-acting beta2-agonist) requests. With new guidelines that discourage overreliance on SABA, asthma expert A/Prof Rigby explains how pharmacists should manage these situations.
What do the new asthma guidelines say?
In the updated NAC Australian Asthma Handbook, released in September 2025, a key guideline change is that no adult or adolescent with asthma should be using salbutamol alone.
‘Every [adult or adolescent] with confirmed asthma now needs to be on an inhaled corticosteroid (ICS),’ A/Prof Rigby said.
The National Asthma Council recently released data that found there were 478 asthma-related deaths in 2024, equating to more than one per day.
There was a surprising increase in asthma deaths in the youngest patient cohort, those aged 0 to 35.
‘This is largely due to poorly controlled asthma, including people over-relying on SABA, not using preventers, or not using anti-inflammatory reliever therapy,’ Ms Rigby said. ‘Those with more severe symptoms should be on maintenance-and-reliever therapy, or MART.’
But that doesn't mean pharmacists should deny patients salbutamol, particularly during events such as storms that can trigger exacerbations.
‘Absolutely supply it if a patient has symptoms – it’s potentially life-saving during an acute episode – but we should be alluding to the fact that it’s risky to use salbutamol alone in asthma,’ she said. ‘‘Use it as an opportunity to explain that the guidelines have changed and that we now have better treatment, but also assess them to determine if they need to see a GP straightaway or go to ED.’
For example, if a patient can’t finish a sentence without taking a breath, they need immediate treatment.
Pharmacists should also remind patients that they should have an asthma action plan, which many adults don’t have. ‘Most people can manage with salbutamol in an acute situation – but they can also use budesonide-formoterol.’
It’s also important to point out the benefits of preventative and anti-inflammatory therapy, including improved asthma control and long-term health outcomes.
‘ICS–formoterol reduces the risk of severe episodes, it's more convenient because you only carry one inhaler and even has environmental benefits,’ A/Prof Rigby said. ‘There are about 15 million salbutamol inhalers used annually, which is a significant carbon footprint.’
What can pharmacists do?
A lot has been learned since the 2016 thunderstorm asthma event, A/Prof Rigby said.
‘The Victoria Department of Health has been very proactive with the pollen-alert apps that give daily high-pollen warnings,’ she said.
There are also similar systems in other states; these apps provide a daily alert using a traffic-light system across mapped regions.
‘For example [on Thursday], the Mildura area was “red” – very high pollen count,’ A/Prof Rigby said.
‘I encourage all pharmacists to sign up, but also to recommend them to patients with asthma and/or allergic rhinitis. When your area is on medium or high alert, pharmacists should be having conversations with patients about being prepared.’
This includes always having a reliever on hand – either salbutamol, or preferably, the anti-inflammatory reliever budesonide-formoterol.
‘During thunderstorm asthma – the “perfect storm” of high pollen plus thunderstorms – people should also avoid being outside, close windows, use air-conditioning, and in cars set air recirculation mode,’ she said.
And when patients present to the pharmacy for treatment for allergic rhinitis, pharmacists should ask: Do you have asthma?
‘Around 80% of people with asthma also have allergic rhinitis, and 40–60% of people with allergic rhinitis also have asthma,’ A/Prof Rigby said. ‘We need to think about “one airway, one disease.” If you get the nose under control, you get better asthma control – and vice versa.’
What’s the approach when it’s not asthma?
During the 2016 thunderstorm asthma event, many people who presented to pharmacies or EDs didn’t have diagnosed asthma, A/Prof Rigby said.
‘Many had hay fever or allergic rhinitis,’ she said. ‘So when people request hay fever treatments, pharmacists should ask about symptoms – such as shortness of breath, cough or chest tightness – which could indicate asthma.’
When these incidents occur, pharmacists should ask whether patients had childhood asthma, hay fever or other respiratory issues. They can also provide Asthma first aid.
‘You can supply a salbutamol puffer – ideally with a spacer – because when people are short of breath they’re less able to coordinate inhalation, and most people don’t use puffers correctly anyway,’ she said.
Pharmacists should use the 4x4x4 method: 4 puffs, one at a time, via a spacer; wait 4 minutes; repeat as needed.
‘If the patient is still short of breath, seek medical advice,’ A/Prof Rigby added. ‘And document everything.’
Pharmacists should also follow-up via phone, text or the next visit.
How should COPD be managed in a storm?
While asthma is reversible with good control, chronic obstructive pulmonary disease (COPD) involves persistent airway inflammation and irreversible obstruction.
Salbutamol may be used to relieve symptoms in patients with COPD, but it does not provide the same level of relief as it does in asthma, A/Prof Rigby said.
‘The perceived benefit of SABA for patients with COPD is often due to the person stopping and resting, or the anxiety relief of “doing something” – rather than actual bronchodilation,’ she said.
But patients with COPD are less likely to have their symptoms triggered by storms.
‘They may be short of breath at rest and have reduced exercise tolerance, so they must take preventative therapy regularly,’ A/Prof Rigby said.
This includes regular use of a long-acting muscarinic antagonist and long-acting beta2-agonist.
‘Only some patients need triple therapy,’ she added.
[post_title] => Severe spring storms show the risks of SABA overuse
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => severe-spring-storms-show-the-risks-of-saba-overuse
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-01 17:45:42
[post_modified_gmt] => 2025-12-01 06:45:42
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31010
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Severe spring storms show the risks of SABA overuse
[title] => Severe spring storms show the risks of SABA overuse
[href] => https://www.australianpharmacist.com.au/severe-spring-storms-show-the-risks-of-saba-overuse/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31013
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31004
[post_author] => 3410
[post_date] => 2025-12-01 11:40:10
[post_date_gmt] => 2025-12-01 00:40:10
[post_content] => Renal expert Carla Scuderi explains the lifelong care journey pharmacists provide to kidney disease patients.
Why specialise in kidney care?
I think kidney health chose me! I was hoping to specialise in a clinical area when a job in the Kidney Health Service came up at the Royal Brisbane and Women’s Hospital. I didn’t know what I was getting myself into, but I couldn’t believe my luck. Here was an area of specialised care in an acute hospital setting with all the feels of community pharmacy. Working in kidney health means providing cradle-to-grave care. You build long-term relationships with patients and support them through key life stages – from family planning to kidney failure and palliative care. Much of the work involves ambulatory care – comprising outpatient clinics, acute or satellite hospital dialysis settings, or home-based therapy – as well as acute inpatient admissions.
What does a kidney specialist do?
Provide medicines advice to patients and the entire multidisciplinary team and ensure medicines are available in each off-site dialysis area while coordinating the pharmacy team across these areas. This might be a visit to a dialysis unit to review new patients or a one-on-one patient consult in the clinic, followed by a consultation with the multidisciplinary team about medicine-related issues. It could also cover admissions in the emergency department through to ward rounds and reviews. Medicines access, tolerability, affordability and polypharmacy are big issues for patients with kidney disease. We also work closely with dietitians, social workers, nurses and nurse practitioners, and nephrologists.
How can community pharmacists help to identify CKD?
Over 2 million Australians are living with kidney disease and fewer than 10% of patients with chronic kidney disease (CKD) are aware they have it. Kidney Health Australia has a great handbook outlining the management of CKD in primary care, with community pharmacists being hugely important in encouraging people to get tested and supporting the lifestyle changes required to reduce the progression of CKD, such as smoking cessation.
Pharmacists can also ask patients when they last had their kidneys checked; particularly anyone with high blood pressure or diabetes. For example, if you offer blood pressure monitoring and the reading is high, ask about the kidneys. Some community pharmacies even have access to point-of-care kidney function estimation devices – brilliant!
What’s the future role of pharmacists in kidney care?
It’s an exciting time to be working in kidney care. New drugs such as sodium-glucose co-transporter 2 inhibitors, glucagon-like peptide-1 receptor agonists and non-steroidal mineralocorticoid receptor antagonists are emerging as superstars in slowing the progression of CKD. I think the future will be much more closely linked with cardiology and metabolic health rather than exclusively kidneys. The link between cardiac disease and kidney health has been given the name cardiovascular-kidney-metabolic (CKM) syndrome. Increasingly, we are using the same drugs to treat all three conditions. I also think pharmacogenomics will play a role in determining which patients are not suited to certain blood pressure medicines, for example, which will help to improve patient outcomes. Hopefully, the future will bring less reliance on dialysis, earlier diagnosis and more successful transplants – allowing people to live well and slowing the progression of CKD.
Any advice for pharmacists keen on specialising in kidney care?
Look for opportunities in adjacent fields such as cardiology and general medicine to build your knowledge. Clinical review skills, ability to perform home medicines reviews and good general drug knowledge are all essentials. You should also prepare to be confronted with blood; watching patients being put onto the dialysis machines can be confronting, particularly if you are queasy. And develop great people skills, because you’ll be with these patients for the long haul. But give it a go, it’s fantastic.
A Day in the life of Carla Scuderi, Assistant Director of Pharmacy Clinical, Royal Brisbane and Women’s Hospital, Brisbane, QLD
| 7.30 am | Early start First job of the day is to coordinate the team and manage any staffing shortfalls. Attend the hospital executive huddle to get an idea of what the day looks like, including planned admissions, surgery and discharges. |
| 8.30 am | Outpatient clinic Transplant clinic is my go-to as these patients have very complex immunosuppressant regimens and medication adherence is paramount. Ensuring we have the drug levels right and making sure patients are managing their other comorbidities, such as hypertension and diabetes, is critical. I review their pathology, weight, blood pressure, dispensing history, self-reported adherence and adverse effects – providing an updated medication list to assist with dose administration aid packing. |
| 11.00 am | Morbidity and mortality meeting Monthly all service line review of patient deaths and unexpected outcomes. This is an opportunity to review patient care, ensure systems are working appropriately and apply learnings to improve outcomes. From a pharmacy perspective, this can include ensuring access to medicines was timely. |
| 1.00 pm | Lunchtime grand rounds Lunchtimes are spent learning with the team. One of the best parts of being part of a big institution is hearing what all the other parts of the hospital do. This week grand rounds were presented by the endocrinology department, who outlined a trial on thyroid replacement treatments. |
| 2.00 pm | Statewide Renal Network meeting Weekly catch up with the Statewide coordinator and my co-chair, a nephrologist in Cairns. There’s an issue regarding potential out-of-stock supplies of a component required for dialysis. Fortunately, we discover that there isn’t a stock shortage, merely a distribution issue. |
| 4.30 pm | Home duties begin Serve as an Uber driver for the teens’ various sport, social or work commitments and ensure the home crew are fed. If I’m lucky, I can sneak in a walk around the Brisbane River or even some laps at the pool. |
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31034
[post_author] => 3410
[post_date] => 2025-12-08 14:06:18
[post_date_gmt] => 2025-12-08 03:06:18
[post_content] => Professor Mark Naunton MPS, Chair of the Faculty of Health and Professor of Pharmacy at the University of Canberra, was unanimously elected by the PSA Board to serve as the next president from January 2026.
The Board has also elected Bridget Totterman MPS as National Vice President (elect) to fill the vacancy created by Prof Naunton’s election.
[caption id="attachment_31037" align="aligncenter" width="600"] Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
What motivated you to seek election as the next PSA National President?
I’ve had a long career in pharmacy, working across academia, research and education – but like most pharmacists, I started in community pharmacy.
As an intern, my preceptor was a PSA branch committee member and he paid for my PSA membership. From the very beginning, it was instilled in me how important it is to give back to the profession.
In research, I saw firsthand the gaps in our healthcare system, which drove me to explore how pharmacists can help to improve care – particularly in transitions of care. I’ve also worked in educational outreach with GPs and pharmacists, showing me how much GPs actually value pharmacists; when we communicate well and have something reasonable to say, they listen. That has always been my experience as a forward-facing clinical pharmacist
My shift into academia was driven by wanting to train the next generation of pharmacists. What I often saw in students wasn’t a lack of knowledge, but a lack of confidence – something I’m keen to address.
A consistent theme throughout my career has been the dedication of pharmacists – and how much more we could achieve with recognition, support and the right structures in place.
I’ve always wanted to use my voice to ensure our profession is heard at the highest level. I believe PSA must continue to lead with strength, vision and, above all, unity – so that our profession can not only cope with change, but thrive through it.
What do you hope to achieve as PSA President?
Recognition and remuneration that truly reflects our expertise as medicines experts are big priorities. We have a highly predominantly female workforce, including PSA’s board. There are pay inequities affecting female pharmacists that must be addressed.
I also want to strengthen PSA’s role as the national leader in pharmacy advocacy. Under Associate Professor Fei Sim’s tenure, PSA has grown significantly in this space, and I want to build on that legacy by ensuring every pharmacist feels supported, valued and confident in their practice.
That includes pharmacists across all settings – from community to hospital, general practice, aged care, academia, industry and government. We need to support and recognise the whole profession.
Fei has been a truly inspirational leader, overseeing the negotiation of the first Strategic Agreement of Pharmacist Professional Practice, establishing the PSA Foundation, driving the strategic agenda for innovation in quality use of medicines, and driving practice forward through her membership of numerous government advisory committees.
[caption id="attachment_31039" align="aligncenter" width="600"] A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
Why do you feel this is such a pivotal moment for PSA and the profession?
The PSA is undergoing a major acquisition of the Australasian College of Pharmacy. Our members voted for it because they believe it’s in the best interests of PSA and the profession, helping us strengthen advocacy, improve our education platform, expand resources, and grow our membership.
Through the acquisition, we also want education and member benefits to become more affordable for pharmacists. Cost-of-living pressures are very real, and we need members to feel that PSA genuinely has their back, making their job easier so they can practise to full scope.
At the same time, healthcare is evolving rapidly. Patients need more accessible and innovative care, with pharmacists uniquely positioned to meet those needs.
Primary care reform is happening now – and this is the moment for PSA to champion pharmacists and ensure we’re at the centre of tomorrow’s healthcare system.
What are the major challenges pharmacists are facing right now?
Workforce sustainability is, and will continue to be a significant issue now and into the near future.
While recognition of our clinical expertise is improving, especially with expanded scope of practice and pharmacist prescribing, it's still new – with awareness and acceptance being ongoing challenges.
COVID-19 highlighted what pharmacists can do exceptionally well, particularly vaccinations.
But pharmacists are stretched, with many competing demands taking a toll. Ensuring pharmacists are properly remunerated and supported is critical to maintaining the sustainability of the profession. My role is to ensure they have a voice at every level.
How do you see the profession evolving in 5 years?
Five years ago, we were doing little more than flu vaccinations. Now we’re administering a much broader range of vaccines nationally. Governments are increasingly looking for more efficient healthcare delivery, and pharmacists have shown we can answer that call. But to continue along this path, we need better-trained pharmacy assistants, because pharmacists can’t do more unless we hand over some tasks.
Another area where we still need to make headway is medicine safety. Pharmacists are trained to ensure patients get the right medicine at the right time, and we have highly skilled pharmacists providing medicines reviews – yet many are constrained by caps and limits that make no sense clinically.
In 5 years’ time, I want to see those barriers gone, so patients can actually receive the expertise pharmacists are ready and willing to provide.
I also want to see pharmacists better integrated into healthcare teams, both physically and digitally. That might mean pharmacists embedded in general practice, or pharmacists who are digitally connected to practices and other care settings. We’re a large country and we know there is a shortage of pharmacists – so we have to find creative ways to connect our expertise to where it’s needed.
How have your background and previous experiences shaped your views of the profession?
I grew up in rural Tasmania and have done a lot of work across rural and regional Australia. I know those communities don’t always feel supported. I understand the challenges facing patients, healthcare workers and pharmacists in those areas, and I want them to know that I hear them.
I’d like people in rural and regional communities to feel they can pick up the phone and talk to me – and to see me as someone who genuinely has their back, just as much as pharmacists in our cities.
I’ve also lived and worked in the Netherlands, where they have often been at the forefront of innovation in data and system design. They have shown what’s possible when you really line up systems to support better care.
I’d like to draw on those experiences and share them with the right people here, because I believe we can learn a great deal from our overseas counterparts as we strengthen pharmacy practice and medicine safety in Australia.
[post_title] => PSA’s new president wants to transform the profession
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => psas-new-president-wants-to-transform-the-profession
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-08 15:16:16
[post_modified_gmt] => 2025-12-08 04:16:16
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31034
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => PSA’s new president wants to transform the profession
[title] => PSA’s new president wants to transform the profession
[href] => https://www.australianpharmacist.com.au/psas-new-president-wants-to-transform-the-profession/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31035
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31020
[post_author] => 3410
[post_date] => 2025-12-03 11:10:54
[post_date_gmt] => 2025-12-03 00:10:54
[post_content] => These case examples show that errors arise from system pressures, not individual failings. Pharmacists can act on these insights to strengthen governance.
When pharmacists call Pharmaceutical Defence Limited (PDL), they’re often navigating some of the most stressful moments of their professional lives.
Behind the scenes, PDL’s professional officers, including pharmacist Claire Bekema – who is also a professional practice pharmacist at PSA – talk pharmacists through clinical decisions, regulatory notifications and incident management.
Here, Ms Bekema outlines the top incidents reported to PDL, alongside practical strategies to reduce risk and respond safely when something goes wrong.
Wrong-patient supply leads to hospital admission
Wrong-patient incidents remain one of the most common and serious error types, often occurring when workflow pressures and assumptions collide.
‘That might be when you call out a script for “[one surname], and somebody just turns up and says, “Yep, that’s me,” and they take it out the door,’ Ms Bekema told participants of PSA’s Voices of Pharmacy – Passion, Purpose, and Possibility webinar last week (26 November).
In one case, which occurred after 60 Day Dispensing was implemented, a patient received two boxes of multiple medicines that were not theirs.
‘It was high-dose antihypertensives, and the patient had low health literacy, so they didn’t know what they were expecting to receive from the doctor,’ she said.
‘They picked up this other person’s medicines and they took one from each box. So they took really high doses of antihypertensives all at once.’
Once errors such as this are discovered, Ms Bekema is clear about what the next steps should be.
‘In this particular scenario, I said, “Let’s talk about the incident and how it occurred later, but the first thing is: try and track down this patient and make sure they’re receiving medical attention”,’ she said.
‘They ended up being transferred to hospital by ambulance because their blood pressure was [extremely low]. Wrong-patient errors can have pretty dire consequences.’
For more information, refer to previous AP coverage on:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31014
[post_author] => 9164
[post_date] => 2025-12-01 15:34:25
[post_date_gmt] => 2025-12-01 04:34:25
[post_content] => The Therapeutic Goods Administration (TGA) has today (Monday 1 December) made updates to product warnings for GLP-1 and dual GIP/GLP-1 receptor agonists for two separate safety issues.
AP examines what pharmacists need to know.
ALERT 1: Potential risk of suicidal thoughts
The TGA has aligned product warnings for all GLP-1 RA medicines to ensure consistent information regarding the potential risk of suicidal thoughts or behaviours.
There have been growing questions about whether there’s a link between GLP-1 RAs and suicidal ideation. As of 23 September 2025, the TGA’s Database of Adverse Event Notifications (DAEN) contains the following:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31010
[post_author] => 3410
[post_date] => 2025-12-01 11:52:12
[post_date_gmt] => 2025-12-01 00:52:12
[post_content] => Australia’s east coast was belted with heavy storms last week. Spring and summer storms can trigger thunderstorm asthma – with bursts of pollen often causing sudden, severe asthma attacks, particularly in patients with asthma or allergic rhinitis.
‘There was the big event in Victoria in November 2016 when 10 people died,’ said Clinical Associate Professor Debbie Rigby FPS, pharmacist and Clinical Executive Lead, National Asthma Council Australia (NAC).
‘But there are other peaks that don’t get as much media coverage – for example, there was terrible weather on Melbourne Cup Day this year, and data showed there were over 100 emergency department (ED) admissions and ambulance callouts that day.’
When asthma symptoms spike, so do SABA (short-acting beta2-agonist) requests. With new guidelines that discourage overreliance on SABA, asthma expert A/Prof Rigby explains how pharmacists should manage these situations.
What do the new asthma guidelines say?
In the updated NAC Australian Asthma Handbook, released in September 2025, a key guideline change is that no adult or adolescent with asthma should be using salbutamol alone.
‘Every [adult or adolescent] with confirmed asthma now needs to be on an inhaled corticosteroid (ICS),’ A/Prof Rigby said.
The National Asthma Council recently released data that found there were 478 asthma-related deaths in 2024, equating to more than one per day.
There was a surprising increase in asthma deaths in the youngest patient cohort, those aged 0 to 35.
‘This is largely due to poorly controlled asthma, including people over-relying on SABA, not using preventers, or not using anti-inflammatory reliever therapy,’ Ms Rigby said. ‘Those with more severe symptoms should be on maintenance-and-reliever therapy, or MART.’
But that doesn't mean pharmacists should deny patients salbutamol, particularly during events such as storms that can trigger exacerbations.
‘Absolutely supply it if a patient has symptoms – it’s potentially life-saving during an acute episode – but we should be alluding to the fact that it’s risky to use salbutamol alone in asthma,’ she said. ‘‘Use it as an opportunity to explain that the guidelines have changed and that we now have better treatment, but also assess them to determine if they need to see a GP straightaway or go to ED.’
For example, if a patient can’t finish a sentence without taking a breath, they need immediate treatment.
Pharmacists should also remind patients that they should have an asthma action plan, which many adults don’t have. ‘Most people can manage with salbutamol in an acute situation – but they can also use budesonide-formoterol.’
It’s also important to point out the benefits of preventative and anti-inflammatory therapy, including improved asthma control and long-term health outcomes.
‘ICS–formoterol reduces the risk of severe episodes, it's more convenient because you only carry one inhaler and even has environmental benefits,’ A/Prof Rigby said. ‘There are about 15 million salbutamol inhalers used annually, which is a significant carbon footprint.’
What can pharmacists do?
A lot has been learned since the 2016 thunderstorm asthma event, A/Prof Rigby said.
‘The Victoria Department of Health has been very proactive with the pollen-alert apps that give daily high-pollen warnings,’ she said.
There are also similar systems in other states; these apps provide a daily alert using a traffic-light system across mapped regions.
‘For example [on Thursday], the Mildura area was “red” – very high pollen count,’ A/Prof Rigby said.
‘I encourage all pharmacists to sign up, but also to recommend them to patients with asthma and/or allergic rhinitis. When your area is on medium or high alert, pharmacists should be having conversations with patients about being prepared.’
This includes always having a reliever on hand – either salbutamol, or preferably, the anti-inflammatory reliever budesonide-formoterol.
‘During thunderstorm asthma – the “perfect storm” of high pollen plus thunderstorms – people should also avoid being outside, close windows, use air-conditioning, and in cars set air recirculation mode,’ she said.
And when patients present to the pharmacy for treatment for allergic rhinitis, pharmacists should ask: Do you have asthma?
‘Around 80% of people with asthma also have allergic rhinitis, and 40–60% of people with allergic rhinitis also have asthma,’ A/Prof Rigby said. ‘We need to think about “one airway, one disease.” If you get the nose under control, you get better asthma control – and vice versa.’
What’s the approach when it’s not asthma?
During the 2016 thunderstorm asthma event, many people who presented to pharmacies or EDs didn’t have diagnosed asthma, A/Prof Rigby said.
‘Many had hay fever or allergic rhinitis,’ she said. ‘So when people request hay fever treatments, pharmacists should ask about symptoms – such as shortness of breath, cough or chest tightness – which could indicate asthma.’
When these incidents occur, pharmacists should ask whether patients had childhood asthma, hay fever or other respiratory issues. They can also provide Asthma first aid.
‘You can supply a salbutamol puffer – ideally with a spacer – because when people are short of breath they’re less able to coordinate inhalation, and most people don’t use puffers correctly anyway,’ she said.
Pharmacists should use the 4x4x4 method: 4 puffs, one at a time, via a spacer; wait 4 minutes; repeat as needed.
‘If the patient is still short of breath, seek medical advice,’ A/Prof Rigby added. ‘And document everything.’
Pharmacists should also follow-up via phone, text or the next visit.
How should COPD be managed in a storm?
While asthma is reversible with good control, chronic obstructive pulmonary disease (COPD) involves persistent airway inflammation and irreversible obstruction.
Salbutamol may be used to relieve symptoms in patients with COPD, but it does not provide the same level of relief as it does in asthma, A/Prof Rigby said.
‘The perceived benefit of SABA for patients with COPD is often due to the person stopping and resting, or the anxiety relief of “doing something” – rather than actual bronchodilation,’ she said.
But patients with COPD are less likely to have their symptoms triggered by storms.
‘They may be short of breath at rest and have reduced exercise tolerance, so they must take preventative therapy regularly,’ A/Prof Rigby said.
This includes regular use of a long-acting muscarinic antagonist and long-acting beta2-agonist.
‘Only some patients need triple therapy,’ she added.
[post_title] => Severe spring storms show the risks of SABA overuse
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => severe-spring-storms-show-the-risks-of-saba-overuse
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-01 17:45:42
[post_modified_gmt] => 2025-12-01 06:45:42
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31010
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Severe spring storms show the risks of SABA overuse
[title] => Severe spring storms show the risks of SABA overuse
[href] => https://www.australianpharmacist.com.au/severe-spring-storms-show-the-risks-of-saba-overuse/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31013
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31004
[post_author] => 3410
[post_date] => 2025-12-01 11:40:10
[post_date_gmt] => 2025-12-01 00:40:10
[post_content] => Renal expert Carla Scuderi explains the lifelong care journey pharmacists provide to kidney disease patients.
Why specialise in kidney care?
I think kidney health chose me! I was hoping to specialise in a clinical area when a job in the Kidney Health Service came up at the Royal Brisbane and Women’s Hospital. I didn’t know what I was getting myself into, but I couldn’t believe my luck. Here was an area of specialised care in an acute hospital setting with all the feels of community pharmacy. Working in kidney health means providing cradle-to-grave care. You build long-term relationships with patients and support them through key life stages – from family planning to kidney failure and palliative care. Much of the work involves ambulatory care – comprising outpatient clinics, acute or satellite hospital dialysis settings, or home-based therapy – as well as acute inpatient admissions.
What does a kidney specialist do?
Provide medicines advice to patients and the entire multidisciplinary team and ensure medicines are available in each off-site dialysis area while coordinating the pharmacy team across these areas. This might be a visit to a dialysis unit to review new patients or a one-on-one patient consult in the clinic, followed by a consultation with the multidisciplinary team about medicine-related issues. It could also cover admissions in the emergency department through to ward rounds and reviews. Medicines access, tolerability, affordability and polypharmacy are big issues for patients with kidney disease. We also work closely with dietitians, social workers, nurses and nurse practitioners, and nephrologists.
How can community pharmacists help to identify CKD?
Over 2 million Australians are living with kidney disease and fewer than 10% of patients with chronic kidney disease (CKD) are aware they have it. Kidney Health Australia has a great handbook outlining the management of CKD in primary care, with community pharmacists being hugely important in encouraging people to get tested and supporting the lifestyle changes required to reduce the progression of CKD, such as smoking cessation.
Pharmacists can also ask patients when they last had their kidneys checked; particularly anyone with high blood pressure or diabetes. For example, if you offer blood pressure monitoring and the reading is high, ask about the kidneys. Some community pharmacies even have access to point-of-care kidney function estimation devices – brilliant!
What’s the future role of pharmacists in kidney care?
It’s an exciting time to be working in kidney care. New drugs such as sodium-glucose co-transporter 2 inhibitors, glucagon-like peptide-1 receptor agonists and non-steroidal mineralocorticoid receptor antagonists are emerging as superstars in slowing the progression of CKD. I think the future will be much more closely linked with cardiology and metabolic health rather than exclusively kidneys. The link between cardiac disease and kidney health has been given the name cardiovascular-kidney-metabolic (CKM) syndrome. Increasingly, we are using the same drugs to treat all three conditions. I also think pharmacogenomics will play a role in determining which patients are not suited to certain blood pressure medicines, for example, which will help to improve patient outcomes. Hopefully, the future will bring less reliance on dialysis, earlier diagnosis and more successful transplants – allowing people to live well and slowing the progression of CKD.
Any advice for pharmacists keen on specialising in kidney care?
Look for opportunities in adjacent fields such as cardiology and general medicine to build your knowledge. Clinical review skills, ability to perform home medicines reviews and good general drug knowledge are all essentials. You should also prepare to be confronted with blood; watching patients being put onto the dialysis machines can be confronting, particularly if you are queasy. And develop great people skills, because you’ll be with these patients for the long haul. But give it a go, it’s fantastic.
A Day in the life of Carla Scuderi, Assistant Director of Pharmacy Clinical, Royal Brisbane and Women’s Hospital, Brisbane, QLD
| 7.30 am | Early start First job of the day is to coordinate the team and manage any staffing shortfalls. Attend the hospital executive huddle to get an idea of what the day looks like, including planned admissions, surgery and discharges. |
| 8.30 am | Outpatient clinic Transplant clinic is my go-to as these patients have very complex immunosuppressant regimens and medication adherence is paramount. Ensuring we have the drug levels right and making sure patients are managing their other comorbidities, such as hypertension and diabetes, is critical. I review their pathology, weight, blood pressure, dispensing history, self-reported adherence and adverse effects – providing an updated medication list to assist with dose administration aid packing. |
| 11.00 am | Morbidity and mortality meeting Monthly all service line review of patient deaths and unexpected outcomes. This is an opportunity to review patient care, ensure systems are working appropriately and apply learnings to improve outcomes. From a pharmacy perspective, this can include ensuring access to medicines was timely. |
| 1.00 pm | Lunchtime grand rounds Lunchtimes are spent learning with the team. One of the best parts of being part of a big institution is hearing what all the other parts of the hospital do. This week grand rounds were presented by the endocrinology department, who outlined a trial on thyroid replacement treatments. |
| 2.00 pm | Statewide Renal Network meeting Weekly catch up with the Statewide coordinator and my co-chair, a nephrologist in Cairns. There’s an issue regarding potential out-of-stock supplies of a component required for dialysis. Fortunately, we discover that there isn’t a stock shortage, merely a distribution issue. |
| 4.30 pm | Home duties begin Serve as an Uber driver for the teens’ various sport, social or work commitments and ensure the home crew are fed. If I’m lucky, I can sneak in a walk around the Brisbane River or even some laps at the pool. |
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31034
[post_author] => 3410
[post_date] => 2025-12-08 14:06:18
[post_date_gmt] => 2025-12-08 03:06:18
[post_content] => Professor Mark Naunton MPS, Chair of the Faculty of Health and Professor of Pharmacy at the University of Canberra, was unanimously elected by the PSA Board to serve as the next president from January 2026.
The Board has also elected Bridget Totterman MPS as National Vice President (elect) to fill the vacancy created by Prof Naunton’s election.
[caption id="attachment_31037" align="aligncenter" width="600"] Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
What motivated you to seek election as the next PSA National President?
I’ve had a long career in pharmacy, working across academia, research and education – but like most pharmacists, I started in community pharmacy.
As an intern, my preceptor was a PSA branch committee member and he paid for my PSA membership. From the very beginning, it was instilled in me how important it is to give back to the profession.
In research, I saw firsthand the gaps in our healthcare system, which drove me to explore how pharmacists can help to improve care – particularly in transitions of care. I’ve also worked in educational outreach with GPs and pharmacists, showing me how much GPs actually value pharmacists; when we communicate well and have something reasonable to say, they listen. That has always been my experience as a forward-facing clinical pharmacist
My shift into academia was driven by wanting to train the next generation of pharmacists. What I often saw in students wasn’t a lack of knowledge, but a lack of confidence – something I’m keen to address.
A consistent theme throughout my career has been the dedication of pharmacists – and how much more we could achieve with recognition, support and the right structures in place.
I’ve always wanted to use my voice to ensure our profession is heard at the highest level. I believe PSA must continue to lead with strength, vision and, above all, unity – so that our profession can not only cope with change, but thrive through it.
What do you hope to achieve as PSA President?
Recognition and remuneration that truly reflects our expertise as medicines experts are big priorities. We have a highly predominantly female workforce, including PSA’s board. There are pay inequities affecting female pharmacists that must be addressed.
I also want to strengthen PSA’s role as the national leader in pharmacy advocacy. Under Associate Professor Fei Sim’s tenure, PSA has grown significantly in this space, and I want to build on that legacy by ensuring every pharmacist feels supported, valued and confident in their practice.
That includes pharmacists across all settings – from community to hospital, general practice, aged care, academia, industry and government. We need to support and recognise the whole profession.
Fei has been a truly inspirational leader, overseeing the negotiation of the first Strategic Agreement of Pharmacist Professional Practice, establishing the PSA Foundation, driving the strategic agenda for innovation in quality use of medicines, and driving practice forward through her membership of numerous government advisory committees.
[caption id="attachment_31039" align="aligncenter" width="600"] A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
Why do you feel this is such a pivotal moment for PSA and the profession?
The PSA is undergoing a major acquisition of the Australasian College of Pharmacy. Our members voted for it because they believe it’s in the best interests of PSA and the profession, helping us strengthen advocacy, improve our education platform, expand resources, and grow our membership.
Through the acquisition, we also want education and member benefits to become more affordable for pharmacists. Cost-of-living pressures are very real, and we need members to feel that PSA genuinely has their back, making their job easier so they can practise to full scope.
At the same time, healthcare is evolving rapidly. Patients need more accessible and innovative care, with pharmacists uniquely positioned to meet those needs.
Primary care reform is happening now – and this is the moment for PSA to champion pharmacists and ensure we’re at the centre of tomorrow’s healthcare system.
What are the major challenges pharmacists are facing right now?
Workforce sustainability is, and will continue to be a significant issue now and into the near future.
While recognition of our clinical expertise is improving, especially with expanded scope of practice and pharmacist prescribing, it's still new – with awareness and acceptance being ongoing challenges.
COVID-19 highlighted what pharmacists can do exceptionally well, particularly vaccinations.
But pharmacists are stretched, with many competing demands taking a toll. Ensuring pharmacists are properly remunerated and supported is critical to maintaining the sustainability of the profession. My role is to ensure they have a voice at every level.
How do you see the profession evolving in 5 years?
Five years ago, we were doing little more than flu vaccinations. Now we’re administering a much broader range of vaccines nationally. Governments are increasingly looking for more efficient healthcare delivery, and pharmacists have shown we can answer that call. But to continue along this path, we need better-trained pharmacy assistants, because pharmacists can’t do more unless we hand over some tasks.
Another area where we still need to make headway is medicine safety. Pharmacists are trained to ensure patients get the right medicine at the right time, and we have highly skilled pharmacists providing medicines reviews – yet many are constrained by caps and limits that make no sense clinically.
In 5 years’ time, I want to see those barriers gone, so patients can actually receive the expertise pharmacists are ready and willing to provide.
I also want to see pharmacists better integrated into healthcare teams, both physically and digitally. That might mean pharmacists embedded in general practice, or pharmacists who are digitally connected to practices and other care settings. We’re a large country and we know there is a shortage of pharmacists – so we have to find creative ways to connect our expertise to where it’s needed.
How have your background and previous experiences shaped your views of the profession?
I grew up in rural Tasmania and have done a lot of work across rural and regional Australia. I know those communities don’t always feel supported. I understand the challenges facing patients, healthcare workers and pharmacists in those areas, and I want them to know that I hear them.
I’d like people in rural and regional communities to feel they can pick up the phone and talk to me – and to see me as someone who genuinely has their back, just as much as pharmacists in our cities.
I’ve also lived and worked in the Netherlands, where they have often been at the forefront of innovation in data and system design. They have shown what’s possible when you really line up systems to support better care.
I’d like to draw on those experiences and share them with the right people here, because I believe we can learn a great deal from our overseas counterparts as we strengthen pharmacy practice and medicine safety in Australia.
[post_title] => PSA’s new president wants to transform the profession
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => psas-new-president-wants-to-transform-the-profession
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-08 15:16:16
[post_modified_gmt] => 2025-12-08 04:16:16
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31034
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => PSA’s new president wants to transform the profession
[title] => PSA’s new president wants to transform the profession
[href] => https://www.australianpharmacist.com.au/psas-new-president-wants-to-transform-the-profession/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31035
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31020
[post_author] => 3410
[post_date] => 2025-12-03 11:10:54
[post_date_gmt] => 2025-12-03 00:10:54
[post_content] => These case examples show that errors arise from system pressures, not individual failings. Pharmacists can act on these insights to strengthen governance.
When pharmacists call Pharmaceutical Defence Limited (PDL), they’re often navigating some of the most stressful moments of their professional lives.
Behind the scenes, PDL’s professional officers, including pharmacist Claire Bekema – who is also a professional practice pharmacist at PSA – talk pharmacists through clinical decisions, regulatory notifications and incident management.
Here, Ms Bekema outlines the top incidents reported to PDL, alongside practical strategies to reduce risk and respond safely when something goes wrong.
Wrong-patient supply leads to hospital admission
Wrong-patient incidents remain one of the most common and serious error types, often occurring when workflow pressures and assumptions collide.
‘That might be when you call out a script for “[one surname], and somebody just turns up and says, “Yep, that’s me,” and they take it out the door,’ Ms Bekema told participants of PSA’s Voices of Pharmacy – Passion, Purpose, and Possibility webinar last week (26 November).
In one case, which occurred after 60 Day Dispensing was implemented, a patient received two boxes of multiple medicines that were not theirs.
‘It was high-dose antihypertensives, and the patient had low health literacy, so they didn’t know what they were expecting to receive from the doctor,’ she said.
‘They picked up this other person’s medicines and they took one from each box. So they took really high doses of antihypertensives all at once.’
Once errors such as this are discovered, Ms Bekema is clear about what the next steps should be.
‘In this particular scenario, I said, “Let’s talk about the incident and how it occurred later, but the first thing is: try and track down this patient and make sure they’re receiving medical attention”,’ she said.
‘They ended up being transferred to hospital by ambulance because their blood pressure was [extremely low]. Wrong-patient errors can have pretty dire consequences.’
For more information, refer to previous AP coverage on:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31014
[post_author] => 9164
[post_date] => 2025-12-01 15:34:25
[post_date_gmt] => 2025-12-01 04:34:25
[post_content] => The Therapeutic Goods Administration (TGA) has today (Monday 1 December) made updates to product warnings for GLP-1 and dual GIP/GLP-1 receptor agonists for two separate safety issues.
AP examines what pharmacists need to know.
ALERT 1: Potential risk of suicidal thoughts
The TGA has aligned product warnings for all GLP-1 RA medicines to ensure consistent information regarding the potential risk of suicidal thoughts or behaviours.
There have been growing questions about whether there’s a link between GLP-1 RAs and suicidal ideation. As of 23 September 2025, the TGA’s Database of Adverse Event Notifications (DAEN) contains the following:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31010
[post_author] => 3410
[post_date] => 2025-12-01 11:52:12
[post_date_gmt] => 2025-12-01 00:52:12
[post_content] => Australia’s east coast was belted with heavy storms last week. Spring and summer storms can trigger thunderstorm asthma – with bursts of pollen often causing sudden, severe asthma attacks, particularly in patients with asthma or allergic rhinitis.
‘There was the big event in Victoria in November 2016 when 10 people died,’ said Clinical Associate Professor Debbie Rigby FPS, pharmacist and Clinical Executive Lead, National Asthma Council Australia (NAC).
‘But there are other peaks that don’t get as much media coverage – for example, there was terrible weather on Melbourne Cup Day this year, and data showed there were over 100 emergency department (ED) admissions and ambulance callouts that day.’
When asthma symptoms spike, so do SABA (short-acting beta2-agonist) requests. With new guidelines that discourage overreliance on SABA, asthma expert A/Prof Rigby explains how pharmacists should manage these situations.
What do the new asthma guidelines say?
In the updated NAC Australian Asthma Handbook, released in September 2025, a key guideline change is that no adult or adolescent with asthma should be using salbutamol alone.
‘Every [adult or adolescent] with confirmed asthma now needs to be on an inhaled corticosteroid (ICS),’ A/Prof Rigby said.
The National Asthma Council recently released data that found there were 478 asthma-related deaths in 2024, equating to more than one per day.
There was a surprising increase in asthma deaths in the youngest patient cohort, those aged 0 to 35.
‘This is largely due to poorly controlled asthma, including people over-relying on SABA, not using preventers, or not using anti-inflammatory reliever therapy,’ Ms Rigby said. ‘Those with more severe symptoms should be on maintenance-and-reliever therapy, or MART.’
But that doesn't mean pharmacists should deny patients salbutamol, particularly during events such as storms that can trigger exacerbations.
‘Absolutely supply it if a patient has symptoms – it’s potentially life-saving during an acute episode – but we should be alluding to the fact that it’s risky to use salbutamol alone in asthma,’ she said. ‘‘Use it as an opportunity to explain that the guidelines have changed and that we now have better treatment, but also assess them to determine if they need to see a GP straightaway or go to ED.’
For example, if a patient can’t finish a sentence without taking a breath, they need immediate treatment.
Pharmacists should also remind patients that they should have an asthma action plan, which many adults don’t have. ‘Most people can manage with salbutamol in an acute situation – but they can also use budesonide-formoterol.’
It’s also important to point out the benefits of preventative and anti-inflammatory therapy, including improved asthma control and long-term health outcomes.
‘ICS–formoterol reduces the risk of severe episodes, it's more convenient because you only carry one inhaler and even has environmental benefits,’ A/Prof Rigby said. ‘There are about 15 million salbutamol inhalers used annually, which is a significant carbon footprint.’
What can pharmacists do?
A lot has been learned since the 2016 thunderstorm asthma event, A/Prof Rigby said.
‘The Victoria Department of Health has been very proactive with the pollen-alert apps that give daily high-pollen warnings,’ she said.
There are also similar systems in other states; these apps provide a daily alert using a traffic-light system across mapped regions.
‘For example [on Thursday], the Mildura area was “red” – very high pollen count,’ A/Prof Rigby said.
‘I encourage all pharmacists to sign up, but also to recommend them to patients with asthma and/or allergic rhinitis. When your area is on medium or high alert, pharmacists should be having conversations with patients about being prepared.’
This includes always having a reliever on hand – either salbutamol, or preferably, the anti-inflammatory reliever budesonide-formoterol.
‘During thunderstorm asthma – the “perfect storm” of high pollen plus thunderstorms – people should also avoid being outside, close windows, use air-conditioning, and in cars set air recirculation mode,’ she said.
And when patients present to the pharmacy for treatment for allergic rhinitis, pharmacists should ask: Do you have asthma?
‘Around 80% of people with asthma also have allergic rhinitis, and 40–60% of people with allergic rhinitis also have asthma,’ A/Prof Rigby said. ‘We need to think about “one airway, one disease.” If you get the nose under control, you get better asthma control – and vice versa.’
What’s the approach when it’s not asthma?
During the 2016 thunderstorm asthma event, many people who presented to pharmacies or EDs didn’t have diagnosed asthma, A/Prof Rigby said.
‘Many had hay fever or allergic rhinitis,’ she said. ‘So when people request hay fever treatments, pharmacists should ask about symptoms – such as shortness of breath, cough or chest tightness – which could indicate asthma.’
When these incidents occur, pharmacists should ask whether patients had childhood asthma, hay fever or other respiratory issues. They can also provide Asthma first aid.
‘You can supply a salbutamol puffer – ideally with a spacer – because when people are short of breath they’re less able to coordinate inhalation, and most people don’t use puffers correctly anyway,’ she said.
Pharmacists should use the 4x4x4 method: 4 puffs, one at a time, via a spacer; wait 4 minutes; repeat as needed.
‘If the patient is still short of breath, seek medical advice,’ A/Prof Rigby added. ‘And document everything.’
Pharmacists should also follow-up via phone, text or the next visit.
How should COPD be managed in a storm?
While asthma is reversible with good control, chronic obstructive pulmonary disease (COPD) involves persistent airway inflammation and irreversible obstruction.
Salbutamol may be used to relieve symptoms in patients with COPD, but it does not provide the same level of relief as it does in asthma, A/Prof Rigby said.
‘The perceived benefit of SABA for patients with COPD is often due to the person stopping and resting, or the anxiety relief of “doing something” – rather than actual bronchodilation,’ she said.
But patients with COPD are less likely to have their symptoms triggered by storms.
‘They may be short of breath at rest and have reduced exercise tolerance, so they must take preventative therapy regularly,’ A/Prof Rigby said.
This includes regular use of a long-acting muscarinic antagonist and long-acting beta2-agonist.
‘Only some patients need triple therapy,’ she added.
[post_title] => Severe spring storms show the risks of SABA overuse
[post_excerpt] =>
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => severe-spring-storms-show-the-risks-of-saba-overuse
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-01 17:45:42
[post_modified_gmt] => 2025-12-01 06:45:42
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31010
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => Severe spring storms show the risks of SABA overuse
[title] => Severe spring storms show the risks of SABA overuse
[href] => https://www.australianpharmacist.com.au/severe-spring-storms-show-the-risks-of-saba-overuse/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31013
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31004
[post_author] => 3410
[post_date] => 2025-12-01 11:40:10
[post_date_gmt] => 2025-12-01 00:40:10
[post_content] => Renal expert Carla Scuderi explains the lifelong care journey pharmacists provide to kidney disease patients.
Why specialise in kidney care?
I think kidney health chose me! I was hoping to specialise in a clinical area when a job in the Kidney Health Service came up at the Royal Brisbane and Women’s Hospital. I didn’t know what I was getting myself into, but I couldn’t believe my luck. Here was an area of specialised care in an acute hospital setting with all the feels of community pharmacy. Working in kidney health means providing cradle-to-grave care. You build long-term relationships with patients and support them through key life stages – from family planning to kidney failure and palliative care. Much of the work involves ambulatory care – comprising outpatient clinics, acute or satellite hospital dialysis settings, or home-based therapy – as well as acute inpatient admissions.
What does a kidney specialist do?
Provide medicines advice to patients and the entire multidisciplinary team and ensure medicines are available in each off-site dialysis area while coordinating the pharmacy team across these areas. This might be a visit to a dialysis unit to review new patients or a one-on-one patient consult in the clinic, followed by a consultation with the multidisciplinary team about medicine-related issues. It could also cover admissions in the emergency department through to ward rounds and reviews. Medicines access, tolerability, affordability and polypharmacy are big issues for patients with kidney disease. We also work closely with dietitians, social workers, nurses and nurse practitioners, and nephrologists.
How can community pharmacists help to identify CKD?
Over 2 million Australians are living with kidney disease and fewer than 10% of patients with chronic kidney disease (CKD) are aware they have it. Kidney Health Australia has a great handbook outlining the management of CKD in primary care, with community pharmacists being hugely important in encouraging people to get tested and supporting the lifestyle changes required to reduce the progression of CKD, such as smoking cessation.
Pharmacists can also ask patients when they last had their kidneys checked; particularly anyone with high blood pressure or diabetes. For example, if you offer blood pressure monitoring and the reading is high, ask about the kidneys. Some community pharmacies even have access to point-of-care kidney function estimation devices – brilliant!
What’s the future role of pharmacists in kidney care?
It’s an exciting time to be working in kidney care. New drugs such as sodium-glucose co-transporter 2 inhibitors, glucagon-like peptide-1 receptor agonists and non-steroidal mineralocorticoid receptor antagonists are emerging as superstars in slowing the progression of CKD. I think the future will be much more closely linked with cardiology and metabolic health rather than exclusively kidneys. The link between cardiac disease and kidney health has been given the name cardiovascular-kidney-metabolic (CKM) syndrome. Increasingly, we are using the same drugs to treat all three conditions. I also think pharmacogenomics will play a role in determining which patients are not suited to certain blood pressure medicines, for example, which will help to improve patient outcomes. Hopefully, the future will bring less reliance on dialysis, earlier diagnosis and more successful transplants – allowing people to live well and slowing the progression of CKD.
Any advice for pharmacists keen on specialising in kidney care?
Look for opportunities in adjacent fields such as cardiology and general medicine to build your knowledge. Clinical review skills, ability to perform home medicines reviews and good general drug knowledge are all essentials. You should also prepare to be confronted with blood; watching patients being put onto the dialysis machines can be confronting, particularly if you are queasy. And develop great people skills, because you’ll be with these patients for the long haul. But give it a go, it’s fantastic.
A Day in the life of Carla Scuderi, Assistant Director of Pharmacy Clinical, Royal Brisbane and Women’s Hospital, Brisbane, QLD
| 7.30 am | Early start First job of the day is to coordinate the team and manage any staffing shortfalls. Attend the hospital executive huddle to get an idea of what the day looks like, including planned admissions, surgery and discharges. |
| 8.30 am | Outpatient clinic Transplant clinic is my go-to as these patients have very complex immunosuppressant regimens and medication adherence is paramount. Ensuring we have the drug levels right and making sure patients are managing their other comorbidities, such as hypertension and diabetes, is critical. I review their pathology, weight, blood pressure, dispensing history, self-reported adherence and adverse effects – providing an updated medication list to assist with dose administration aid packing. |
| 11.00 am | Morbidity and mortality meeting Monthly all service line review of patient deaths and unexpected outcomes. This is an opportunity to review patient care, ensure systems are working appropriately and apply learnings to improve outcomes. From a pharmacy perspective, this can include ensuring access to medicines was timely. |
| 1.00 pm | Lunchtime grand rounds Lunchtimes are spent learning with the team. One of the best parts of being part of a big institution is hearing what all the other parts of the hospital do. This week grand rounds were presented by the endocrinology department, who outlined a trial on thyroid replacement treatments. |
| 2.00 pm | Statewide Renal Network meeting Weekly catch up with the Statewide coordinator and my co-chair, a nephrologist in Cairns. There’s an issue regarding potential out-of-stock supplies of a component required for dialysis. Fortunately, we discover that there isn’t a stock shortage, merely a distribution issue. |
| 4.30 pm | Home duties begin Serve as an Uber driver for the teens’ various sport, social or work commitments and ensure the home crew are fed. If I’m lucky, I can sneak in a walk around the Brisbane River or even some laps at the pool. |
Get your weekly dose of the news and research you need to help advance your practice.
Protected by Google reCAPTCHA v3.

Australian Pharmacist is the official journal for Pharmaceutical Society of Australia Ltd.