AP spoke to six pharmacists about their pandemic experiences and the next hurdles that are expected.
As Australia starts its transition through the national plan to reopen to the world, the race to vaccinate all Australia continues apace.
After coming all this way – through aggressive suppression and then a massive fast-tracking of the vaccine rollout following a sluggish start with drastic supply issues – an end, of sorts, is in sight.
While the people of New South Wales, Victoria and the ACT grapple with restrictions that accompany freedoms permitted with the full vaccination of 80% and 90% of their eligible populations, are we at last looking at COVID-normal?
It remains for the rest of the country to catch up to a national average of 80% when full international and domestic travel will resume and life will continue, albeit ‘living with COVID’ that poses a threat to those who remain unvaccinated.
Last month, as Victoria broke through the 2,000+ daily infection ceiling for the first time, its acting Chief Health Officer, Professor Ben Cowie pointed to the success of vaccination in suppressing hospitalisations as well as ‘orders of magnitude’ of cases. While 5% of cases became hospitalised, that was half of the hospitalisations during the winter of 2020 when no vaccines were available, Melbourne locked down for 4 months and hundreds died.
The differing experiences of six pharmacists around the country on the pages following, reflect on how practices have changed since mid-last year.
While half the country this year has been largely unaffected by COVID-19 cases, life in the south-east of the country, particularly community and hospital pharmacists in some cities, towns and rural areas like Walgett and Wilcannia in NSW, has been vastly changed. Last year, virus suppression measures included constantly changing regulations, sanitising, fear of fomites, multiplying sneeze screens and deep cleaning, social distancing, and stopping consumers at store fronts.
This year airborne infection risk and close contact indoors and within households was the focus. The arrival of the Delta strain in Sydney in June made imperative the need for vaccinations which were on a slow rollout with multiple problems including supply issues.
‘Every time someone gets vaccinated will increase the protection for the entire community. That’s what the Doherty modelling shows clearly,’ says Australian Government Deputy Chief Medical Officer, Professor Michael Kidd.1 ‘Vaccinations have increased significantly and we are fast approaching the rates where we can reopen as a nation.’
‘The National Plan to Transition Australia’s National COVID-19 Response2 outlines the Government’s policy framework for safely reopening, consistent with health advice.’ The 4-phase plan, released as NSW entered what would be a 15-week lockdown with a daily high of 1,599 infections – eclipsed by Victoria’s more than 2,297 weeks later – involves transitioning phases A and B (see Table 1) and stepping through phases C and D to at least 80% of the national population vaccinated and living a new normal with the virus in the community, like influenza, which is not far away
The plan was based on modelling for National Cabinet by Melbourne’s Doherty Institute that concluded the country can open up with 80% of the total population vaccinated, but with the pandemic to be regarded as a ‘fire’ to be fought on multiple fronts.3 The 70% national vaccination milestone was reached last month.
Professor Lisa Nissen, Head of the School of Clinical Sciences at Queensland University of Technology and pharmacist member of the Immunisation Landscape subgroup of the Australian Technical Advisory Group on Immunisation (ATAGI) Working Group, says Australia has found itself in an interesting position in the COVID-19 race. ‘Taking fast and effective public health measures early … limited the impact of the virus in the community – effectively buying time to prepare, protect and educate the community about the impact of the disease.
‘However,’ she says, ‘the unintended consequence is that we have in essence created an environment that is vaccine naïve, limited in its “real” experience of the virus and impact on people and the health system and therefore somewhat resistant [earlier] to the drive to get vaccinated.’ Added to this, and the 3-month delay in getting pharmacists involved, was ‘a very slow vaccine rollout’ with supply limitations, controls on who could be vaccinated, poor media and communications on the adverse events related to AstraZeneca vaccines effectively stalling the rollout for up to 4 months when ‘people lost interest, got frustrated and gave up. We almost had to start again.’
Table 1 – Extract from the National Plan to transition Australia’s National COVID-19 Response
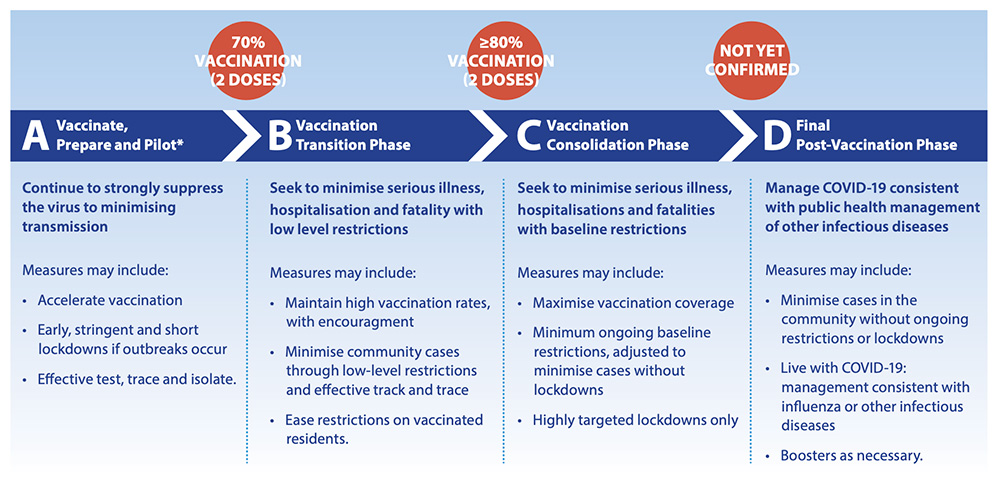
*No jurisdiction required. To increase restrictions beyond current settings. The Plan is based on the current situation and is subject to change if required The COVID-19 Risk Analysis and Response Taskforce’s report is available at: pmc.gov.au
Professor Nissen maintains that maximising vaccination access to CALD, First Nations, refugee, homeless and other vulnerable groups ‘is key’.
In addition to recommending mRNA vaccines for 12–15-year-old children, with an astonishing uptake with the help of pharmacists since September, ATAGI last month recommended third primary doses of a COVID-19 vaccine for severely immunocompromised populations.4
ATAGI is currently considering an application by Pfizer to dose children aged 5–11. And booster shots for the general population have been purchased, with parts of that rollout (aged care) poised to start shortly.

Meagan Gunn MPS, Senior Pharmacist, Orana Mall Pharmacy, Dubbo, NSW
Life changed dramatically for Mrs Gunn when the Dubbo region went into lockdown for 2 months from 11 August following an outbreak.
Last year, when COVID hardly touched large swathes of regional NSW, and Dubbo had a mere handful of cases linked to a cruise ship, the major focus was on hand sanitising, social distancing and home deliveries. But with the recent outbreak, thousands of residents in the Central West NSW region waiting up to 4 hours for COVID-19 tests, it was inevitable that positive cases would impact Mrs Gunn’s pharmacy posing a risk to staff and their families.
By September 26 more than 35,000 people in the Dubbo Regional Council local government area had been tested and pharmacists were in full PPE (gown, gloves, mask and shield) with limited interaction (less than 15 minutes in confined spaces) where possible.
‘The town has worked together to get vaccination rates higher and adhere to the public health orders. Our phones ran hot with vaccination inquiries and bookings,’ she says. Workloads at the pharmacy, open 60 hours a week, increased significantly as positive
case numbers rose above 500, with a significant impact on the Aboriginal population as well as two residential aged care facilities.
PPE-clad staff home-delivered medicines and essential supplies for up to 6 hours a day. A contactless direct-to-car option was offered. Professional services expanded – administering more than 1,500 COVID-19 vaccines. With an ever- changing environment, ‘we have adapted and changed our practices quickly’, Mrs Gunn says. Staff were tested and isolated at home several times after a COVID-19 patient visited the pharmacy. Rosters changed quickly and work reprioritised.
‘As the state reopens and we move to the next phase, the health system will no doubt be under great pressure, both with COVID and with non-COVID-related care,’ Mrs Gunn says. ‘Many people have had elective surgeries deferred and others delayed essential medical tests and screening. Our pharmacy will continue to provide a high level of professional service, encourage contactless delivery where applicable and support e-scripts to assist in minimising community transmission.’
David Sun MPS, Owner, Cincotta Discount Chemist, Auburn, NSW
In the 18 months since COVID-19 arrived in Australia David Sun has noticed a vast change in the resilience of his staff.
His pharmacy, in the south-western Sydney suburb of Auburn, has been through two lockdowns – one last year and this year’s for more than 3 months.
‘Last year the staff were very worried and some asked for leave or time off, but this year with the [Delta strain] outbreak far more serious, none of my staff have asked for leave,’ he says. Auburn was one of the Sydney suburbs at the epicentre of coronavirus infections, within a Local Government Area of concern, which peaked from July to September. Residents were ordered by the NSW Government into a hard lockdown of stay-at-home orders, night-time curfews and police patrols.
Customers were scared to be out in public and the volume of pharmacy home deliveries – ‘even of Panadol’ – increased three-fold compared to last year, Mr Sun says. His pharmacy had to develop safety protocols due to the lack of official guidelines provided by state and federal governments. Staff were positioned near the pharmacy entrance to conduct temperature checks on customers, ensure they used the QR codes and only stayed in the shop for 15 minutes. Then they split into rotating teams, a crucial decision when an infected customer in the pharmacy sent the six members of Team A into isolation for 14 days, leaving Team B to operate the pharmacy.
From August the pharmacy started administering vaccinations, initially expecting 20 patients a day but demand quickly surged to 50 a day.
And at the end of August Mr Sun welcomed new son, Jayden, and took some well-earned leave to help his wife and care for their energetic toddler son, Ethan. ‘It’s been a busy year.

Kevin Ngo MPS, pharmacist manager, Direct Chemist Outlet, Naracoorte, SA
For pharmacists in states with zero or few COVID-19 cases up to this year, much time has been spent encouraging vaccinations and educating the vaccine hesitant.
Kevin Ngo says the residents in Naracoorte, 336 kilometres south-east of Adelaide, had been ‘happy to roll up their sleeves to get vaccinated’, but there had been many discussions with consumers fearful of vaccine adverse effects who were confused by changing advice and misinformation on social media.
‘We have found that explaining to the patient the risk factors of the adverse effects [vs getting COVID-19] and providing them with reassurance is key to encouraging greater uptake.
Health professionals, he says, are constantly monitoring advice from governments and regulatory bodies, including mandatory vaccination of healthcare workers in all states.

Sarah Risdale, Clinical Pharmacist, Royal Brisbane and Women’s Hospital
Working in a COVID-19 ward this year has been a unique, challenging and rewarding experience, for Ms Risdale.
‘The COVID pharmacist is just like any other, working closely with all teams on the ward to contribute to patient care and medicine management but separated from the main hospital (as part of the COVID bubble) which can be isolating both social and professionally at times. It can
be a challenge to complete everyday tasks such as discharge planning or face-to-face medication histories, so I have had to find innovative ways to engage with patients including teams phone and video calls, and room intercoms,’ Ms Risdale says.
‘One of the real eye-opening moments was seeing a COVID-19 pneumonitis X-ray for the first time and realising just how quickly patients could deteriorate and fatigue,’ she says.
And the PPE was challenging. ‘I often joke that 1 week in normal life is about
4 in COVID land because of how rapidly things can change. The hospital as a whole has been very good at monitoring and reacting to changes in the local, national and international situations.
‘We were lucky enough to have pharmacists involved right from the very start of the vaccination roll out earlier this year – in both production and immunisation roles. ‘
An important part of my role as a pharmacist immuniser in our clinic centred around engaging in conversations with people around their fears and concerns about vaccination and providing education and reassurance to help them make informed choices,’ Ms Risdale says.
When COVID-19 comes to Queensland, the time and effort of constant planning will ‘ensure we have a very ready and capable workforce’. With so much research on COVID treatments, ‘it’s easy to get confused or misled’, she says. ‘The National COVID-19 Clinical Evidence Taskforce’s living guidelines is my go-to for the most up-to-date, evidence-based recommendations. It has great flow charts for treatments and I find it clearly explains evidence behind the recommendations.’
Masks, she believes, will be around ‘for a while’, perhaps in long-term use on flights and at airports and the obvious baseline public health measures such as vaccination, good hand hygiene practices and staying home when sick, should remain in high-risk settings such as healthcare. And boosters/annual vaccination will also help lower disease burden and community transmission.
‘We are already starting to see the mental health impacts … but I think it will be a while before we see the true impacts of deferred healthcare,’ she says, such as yearly eye and dental checks, mammograms and skin checks.
Quoc an Sam MPS, Owner, Acher Pharmacy, Flemington, Victoria
Acher Pharmacy had early experience as an emergency service when a nearby public housing tower in the inner Melbourne suburb of Flemington was locked down in July 2020 to contain a COVID-19 outbreak.
Mr Sam’s 18 staff were stressed and fearful with the infection source so close as they delivered medicines to residents in the public housing tower.
‘We had to barricade the shopfront to prevent clients coming into the pharmacy and were running up and down from the dispensary to the front to serve customers,’ he recalls. ‘We worked extra hard to supply and deliver medicines to the locked down tower residents with no reimbursement.’
Mr Sam said he was not paid by the Victorian Department of Health and Human Services for medicines supplied. ‘At the moment I am about $800 out of pocket, which I now consider as my personal donation to COVID,’ he says.
‘Customers have had to adapt to the way our shop operates, like waiting outside. It’s a little inconvenient but we are still able to deliver our services,’ Mr Sam says. ‘At least now we know that vaccines do work in preventing the disease and we hope that by achieving a high vaccination rate we can reduce the spread of COVID-19 in the near future.

Ibrahim Zeini MPS, Managing Pharmacist, Coombabah Chempro Chemist, Gold Coast
As Australia moves towards an 80% fully vaccinated rate, Ibrahim Zeini expects vaccine hesitancy will reduce to ensure ‘lockdown freedoms aren’t short-lived’.
While last year vaccinations were a hoped-for solution, this year he has seen widespread hesitancy, particularly during periods of low COVID-19 transmission and ‘a fear of the unknown’ that has been difficult to manage in some parts of the state, which will open fully next month.
‘A large portion of our community members are already fully vaccinated and we are seeing a rise in unvaccinated people coming in for their first shot.
‘I am confident this would assist us in managing an outbreak effectively.’ ‘While vaccination is the only way forward, it is human nature to resent and rebel when being forced to comply.’ ‘The onus of responsibility should be with frontline healthcare professionals to empower and guide [patients] into making an informed decision. They are … integral to reducing community transmission.’
Next year, after a rejuvenated summer, he hopes to be back to an altered ‘normal’, with boosters ready.
End of race or first lap?
With the worst over, but a long way to go, ‘everyone, particularly pharmacists in a prime position in the community, will be critical in continuing the health messages and providing clear and assessable information’ in future,’ says Prof Nissen.
And there is no reason not to see ‘multiple brands’ of vaccines in pharmacies as they become available, she says.
A schedule for booster vaccines 6 months after a second dose was outlined last month by the federal government. ahead of TGA approval.5
With the imminent start of boosters, it makes sense that much of the ongoing management of COVID-19 vaccination in the future will be in primary care,’ Prof Nissen says.
‘And having spent some time in the [ATAGI] taskforce, I would say that pharmacists have multiple contributions to make – well beyond ordering syringes and fridges … Pharmacists should and could be involved at all levels and from the beginning of planning.
‘Policy, legislation, workforce, training, consumer and stakeholder engagement, work/clinic models, clinical protocols, logistics – these are all things I have done, and more.’
And as Prof Kidd says: ‘We are now in that critical juncture where Australia is learning to live with COVID-19’, with rates of first doses climbing past 80% and NSW, ACT and Victoria open ahead of other states. ‘Vaccination is the key for us to move forward with the national plan and to get people protected.‘
After that, COVID-19 will be primarily self-managed or managed in primary care as it becomes an endemic disease. As more treatments emerge, including four already on order, for most of Australia and the world while the hardest lap is complete, we are still in a marathon.
References
- Doherty Institute. Doherty modelling report revised 10th August 2021. At: www.doherty.edu.au/uploads/content_doc/DohertyModelling_NationalPlan_and_Addendum_ 20210810.pdf
- Australian Government. National plan to transition Australia’s national COVID-19 response. 2021. At: www.pm.gov.au/sites/ default/files/media/national-plan-060821_0.pdf
- Doherty Institute. Statement on the Doherty Institute modelling. 18 September 2021. At: www.doherty.edu.au/news-events/ news/doherty-institute-modelling-report-for-national- cabinet-sep-18
- Australian Government Department of Health.ATAGI. Recommendation on the use of a 3rd primary dose of COVID-19 in individuals who are severely immunocompromised. 2021.
At: https://www.health.gov.au/sites/default/files/ documents/2021/10/atagi-recommendations-on-the-use-of-a- third-primary-dose-of-covid-19-vaccine-in-individuals-who-are- severely-immunocompromised_1.pdf - Ministers, Department of Health. Mininster Hunt’s press conference in Canberra on the vaccination rollout, vaccine booster update, stem cell mission grants, booster program and net zero emissions policy. At: https://bit.ly/3pofelM



 John Jones MPS, pharmacist immuniser and owner of My Community Pharmacy Shortland in Newcastle, NSW[/caption]
John Jones MPS, pharmacist immuniser and owner of My Community Pharmacy Shortland in Newcastle, NSW[/caption]


 Debbie Rigby FPS explaining how to correctly use different inhaler devices[/caption]
Debbie Rigby FPS explaining how to correctly use different inhaler devices[/caption]




 Professor Sepehr Shakib[/caption]
Professor Sepehr Shakib[/caption]

 Lee McLennan MPS[/caption]
Lee McLennan MPS[/caption]
 Dr Natalie Soulsby FPS, Adv Prac Pharm[/caption]
Dr Natalie Soulsby FPS, Adv Prac Pharm[/caption]
 Joanne Gross MPS[/caption]
Joanne Gross MPS[/caption]