

td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31089
[post_author] => 3387
[post_date] => 2025-12-15 16:54:53
[post_date_gmt] => 2025-12-15 05:54:53
[post_content] => New year, new policy and practice changes. Here’s what pharmacists will need to navigate from January.
In 2026, pharmacists can expect some changes to education, medicine costs and credentialing standards.
AP has rounded up the key changes pharmacists can expect from 1 January.
1. PBS co‑payment will drop
From 1 January 2026, the maximum Pharmaceutical Benefits Scheme (PBS) co‑payment for general patients will drop from $31.60 to $25.00 per prescription.
This marks a major reduction in out-of-pocket costs for Australians without a concession card, and the first time in more than 20 years that PBS medicines will cost no more than $25.
However, indexation on the general patient co-payment will resume in 2027 in line with the Consumer Price Index (CPI). Although PBS medicines will not be permanently capped at $25, the long‑term trajectory of general patient co‑payments will rise from a much lower baseline.
2. Transition to the new MMR credential must be completed
By 1 January 2026, pharmacists must have transitioned to the APC’s new Medication Management Review credential to continue:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31095
[post_author] => 9164
[post_date] => 2025-12-15 13:10:40
[post_date_gmt] => 2025-12-15 02:10:40
[post_content] => The Pharmaceutical Society of Australia (PSA) recently launched the PSA Standards for Continuing Professional Development (CPD) for Pharmacists, marking a new era for the accreditation of CPD activities for the pharmacy profession.
The launch of the PSA Standards follows the retirement of the Australian Pharmacy Council (APC) Accreditation Standards for CPD Activities on 31 December 2025. Developed through extensive consultation with the profession, the PSA Standards provide a contemporary framework to guide the quality and educational integrity of continuing professional development activities for pharmacists.
With the commencement of these Standards, CPD providers can apply for accreditation under the PSA Accredited CPD framework.
All supporting materials, including application forms and the PSA Accredited CPD Provider Handbook, will be available on the PSA website from 5 January 2026.
PSA acknowledges and thanks the individuals and organisations who contributed feedback during the consultation process and looks forward to supporting providers in delivering high-quality education for pharmacists.
PSA National President Associate Professor Fei Sim FPS reflected on the process of developing the Standards, acknowledging the work of all involved, including the individuals and organisations who provided feedback during the consultation period.
“The approval of the PSA standards for CPD for pharmacists marks a significant milestone in PSA’s already rich history in upholding quality education standards, now spanning decades,” she said.
“We know our education and continuing professional development are core values for our members. I want to assure you that these standards will give pharmacists the confidence that the CPD they access is of high quality.
“I sincerely thank everyone who participated in the consultation process. It is an incredible achievement to be sharing this news only 5 months after announcing PSA’s intent to publish these education standards.”
To view the Standards or enquire about the accreditation process, please visit https://www.psa.org.au/cpd/
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 30937
[post_author] => 250
[post_date] => 2025-12-10 12:05:46
[post_date_gmt] => 2025-12-10 01:05:46
[post_content] => From emergency contraception to migraines, advance supply can be appropriate. Here’s how to decide when it is – and isn’t.
It might sound like an odd request. Someone requesting a Pharmacist Only Medicine (S3) to have on hand for anticipated use in the future, rather than to respond to a current ailment or symptom. Is this allowed? And if so, when is it appropriate?
Is advance provision of S3s legal?
The answer is a (qualified) yes. While one of the primary reasons a medicine may be listed in Schedule 3 of the SUSMP,1 no Australian jurisdiction restricts advance provision of Pharmacist Only Medicines (see table).
But don’t we need to assess a patient’s therapeutic need?
Yes, the pharmacist must be satisfied there is a therapeutic need for the S3 medicine. This is mandated both in the Professional Practice Standards 2023, as well as (most) state and territory poisons regulations.
However, that therapeutic need doesn’t necessarily need to be for immediate treatment.
There will be circumstances where a therapeutic need for future use exists. For example, the APF2 treatment guidelines for emergency contraception, adrenaline and cold sores supports advance provision.
Similarly, there are cases – albeit less frequently – where advance provision is appropriate for treatment of conditions such as migraine, hives, allergic rhinitis or nasal congestion.
So when is advanced supply of S3 OK?
Quite often, but not always. Advance provision is most appropriate where a patient will need the medicine as time-sensitive treatment for a flare-up of a condition or expected recurrence of an ailment.
Advance provision is also more appropriate where a patient is unlikely to have reasonable access to a pharmacy, which is not limited to international travel.
Advance provision may not be appropriate where the patient may not be able to self-assess appropriate treatment for symptoms after counselling, where a therapeutic need does not exist, or if you believe there is a strong risk of diversion (although this is rare).
What other things do I need to consider?
There are a few, including:
These factors should be addressed in discussion with the patient when advance provision occurs.
As an opioid analogue for treatment of dry cough, it will be pretty unlikely a patient will have a reasonable therapeutic need for advance provision of dihydrocodeine syrup.
However, each request should be considered on its own merits. There will be isolated cases where it is appropriate.
| ACT3 | No comparable criteria |
| NSW4 | · pharmacist gives the person an opportunity to seek advice as to the use of the substance · quantity, or for a purpose must accord with the recognised therapeutic standard of what is appropriate in the circumstances |
| NT5 | · pharmacist must not intentionally supply to a person in a manner reckless to their circumstance |
| QLD6 | · pharmacist reasonably believes the patient has a therapeutic need |
| SA | No comparable criteria |
| TAS7 | · pharmacist forms the opinion use in the treatment of the patient is justified on consideration of the condition, disease or symptoms of the person |
| VIC8 | · for treatment of a patient under pharmacist’s care · pharmacist has taken all reasonable steps to ensure a therapeutic need exists |
| WA9 | No comparable criteria |
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31034
[post_author] => 3410
[post_date] => 2025-12-08 14:06:18
[post_date_gmt] => 2025-12-08 03:06:18
[post_content] => Professor Mark Naunton MPS, Chair of the Faculty of Health and Professor of Pharmacy at the University of Canberra, was unanimously elected by the PSA Board to serve as the next president from January 2026.
The Board has also elected Bridget Totterman MPS as National Vice President (elect) to fill the vacancy created by Prof Naunton’s election.
[caption id="attachment_31037" align="aligncenter" width="600"] Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
What motivated you to seek election as the next PSA National President?
I’ve had a long career in pharmacy, working across academia, research and education – but like most pharmacists, I started in community pharmacy.
As an intern, my preceptor was a PSA branch committee member and he paid for my PSA membership. From the very beginning, it was instilled in me how important it is to give back to the profession.
In research, I saw firsthand the gaps in our healthcare system, which drove me to explore how pharmacists can help to improve care – particularly in transitions of care. I’ve also worked in educational outreach with GPs and pharmacists, showing me how much GPs actually value pharmacists; when we communicate well and have something reasonable to say, they listen. That has always been my experience as a forward-facing clinical pharmacist
My shift into academia was driven by wanting to train the next generation of pharmacists. What I often saw in students wasn’t a lack of knowledge, but a lack of confidence – something I’m keen to address.
A consistent theme throughout my career has been the dedication of pharmacists – and how much more we could achieve with recognition, support and the right structures in place.
I’ve always wanted to use my voice to ensure our profession is heard at the highest level. I believe PSA must continue to lead with strength, vision and, above all, unity – so that our profession can not only cope with change, but thrive through it.
What do you hope to achieve as PSA President?
Recognition and remuneration that truly reflects our expertise as medicines experts are big priorities. We have a highly predominantly female workforce, including PSA’s board. There are pay inequities affecting female pharmacists that must be addressed.
I also want to strengthen PSA’s role as the national leader in pharmacy advocacy. Under Associate Professor Fei Sim’s tenure, PSA has grown significantly in this space, and I want to build on that legacy by ensuring every pharmacist feels supported, valued and confident in their practice.
That includes pharmacists across all settings – from community to hospital, general practice, aged care, academia, industry and government. We need to support and recognise the whole profession.
Fei has been a truly inspirational leader, overseeing the negotiation of the first Strategic Agreement of Pharmacist Professional Practice, establishing the PSA Foundation, driving the strategic agenda for innovation in quality use of medicines, and driving practice forward through her membership of numerous government advisory committees.
[caption id="attachment_31039" align="aligncenter" width="600"] A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
Why do you feel this is such a pivotal moment for PSA and the profession?
The PSA is undergoing a major acquisition of the Australasian College of Pharmacy. Our members voted for it because they believe it’s in the best interests of PSA and the profession, helping us strengthen advocacy, improve our education platform, expand resources, and grow our membership.
Through the acquisition, we also want education and member benefits to become more affordable for pharmacists. Cost-of-living pressures are very real, and we need members to feel that PSA genuinely has their back, making their job easier so they can practise to full scope.
At the same time, healthcare is evolving rapidly. Patients need more accessible and innovative care, with pharmacists uniquely positioned to meet those needs.
Primary care reform is happening now – and this is the moment for PSA to champion pharmacists and ensure we’re at the centre of tomorrow’s healthcare system.
What are the major challenges pharmacists are facing right now?
Workforce sustainability is, and will continue to be a significant issue now and into the near future.
While recognition of our clinical expertise is improving, especially with expanded scope of practice and pharmacist prescribing, it's still new – with awareness and acceptance being ongoing challenges.
COVID-19 highlighted what pharmacists can do exceptionally well, particularly vaccinations.
But pharmacists are stretched, with many competing demands taking a toll. Ensuring pharmacists are properly remunerated and supported is critical to maintaining the sustainability of the profession. My role is to ensure they have a voice at every level.
How do you see the profession evolving in 5 years?
Five years ago, we were doing little more than flu vaccinations. Now we’re administering a much broader range of vaccines nationally. Governments are increasingly looking for more efficient healthcare delivery, and pharmacists have shown we can answer that call. But to continue along this path, we need better-trained pharmacy assistants, because pharmacists can’t do more unless we hand over some tasks.
Another area where we still need to make headway is medicine safety. Pharmacists are trained to ensure patients get the right medicine at the right time, and we have highly skilled pharmacists providing medicines reviews – yet many are constrained by caps and limits that make no sense clinically.
In 5 years’ time, I want to see those barriers gone, so patients can actually receive the expertise pharmacists are ready and willing to provide.
I also want to see pharmacists better integrated into healthcare teams, both physically and digitally. That might mean pharmacists embedded in general practice, or pharmacists who are digitally connected to practices and other care settings. We’re a large country and we know there is a shortage of pharmacists – so we have to find creative ways to connect our expertise to where it’s needed.
How have your background and previous experiences shaped your views of the profession?
I grew up in rural Tasmania and have done a lot of work across rural and regional Australia. I know those communities don’t always feel supported. I understand the challenges facing patients, healthcare workers and pharmacists in those areas, and I want them to know that I hear them.
I’d like people in rural and regional communities to feel they can pick up the phone and talk to me – and to see me as someone who genuinely has their back, just as much as pharmacists in our cities.
I’ve also lived and worked in the Netherlands, where they have often been at the forefront of innovation in data and system design. They have shown what’s possible when you really line up systems to support better care.
I’d like to draw on those experiences and share them with the right people here, because I believe we can learn a great deal from our overseas counterparts as we strengthen pharmacy practice and medicine safety in Australia.
[post_title] => PSA’s new president wants to transform the profession
[post_excerpt] => PSA's new President, Professor Mark Naunton MPS, was unanimously elected by the Board to serve as the next president from January 2026.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => psas-new-president-wants-to-transform-the-profession
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-08 16:08:27
[post_modified_gmt] => 2025-12-08 05:08:27
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31034
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => PSA’s new president wants to transform the profession
[title] => PSA’s new president wants to transform the profession
[href] => https://www.australianpharmacist.com.au/psas-new-president-wants-to-transform-the-profession/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31035
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 30876
[post_author] => 10832
[post_date] => 2025-12-06 15:41:09
[post_date_gmt] => 2025-12-06 04:41:09
[post_content] => Case scenario
Leila, a 35-year-old woman, presents to the pharmacy concerned about a painful red bump near the margin of her upper eyelid. She explains that it appeared 2 days ago and has become increasingly tender, but she has not sought any treatment yet. Leila wears contact lenses and applies eye makeup daily. On further questioning, you learn that she is not taking any regular medications, has no underlying medical conditions, and this is the first time she has experienced such symptoms. She asks if there is anything she can apply to help.
Learning objectivesAfter reading this article, pharmacists should be able to:
|
A hordeolum, commonly known as a stye, is a common eyelid condition caused by bacterial infection of the sebaceous glands. There are two main types: external hordeolum, the more common form, which affects glands near the lash line; and internal hordeolum, which involves the meibomian glands deeper within the eyelid. Although typically benign and self-limiting, a stye is among the more common eyelid conditions seen in primary care.1 It can cause significant discomfort and cosmetic concern for patients. Most cases resolve spontaneously, but referral to a medical practitioner may be warranted in certain circumstances.
Styes are a frequent presentation in community practice, where pharmacists are well equipped to provide reassurance, advise on conservative management, reinforce good eyelid hygiene, and recognise when referral is needed. This article provides an overview of the clinical features of styes, outlines referral criteria, explores management strategies, and highlights the important role pharmacists play in supporting patients with this common condition.
An external hordeolum arises from obstruction and secondary infection of the glands of Zeis or Moll, located along the eyelid margin. In contrast, an internal hordeolum is less common and results from infection of the meibomian gland, situated deeper within the tarsal plate of the eyelid. Staphylococcus aureus is the pathogen most frequently implicated, and styes may also occur secondary to blepharitis, a chronic inflammatory condition of the eyelid.2
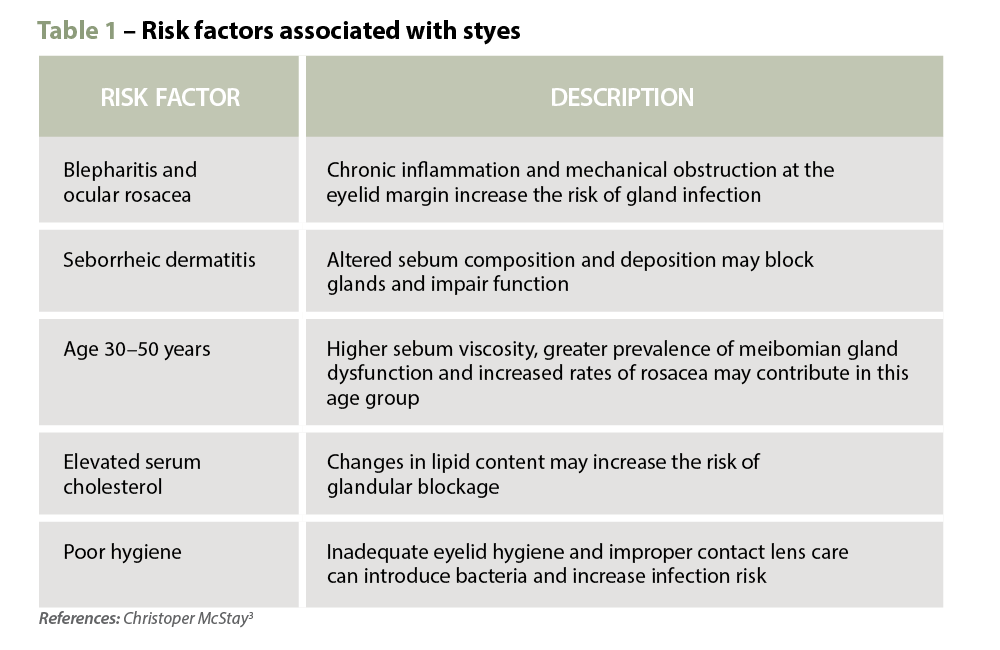
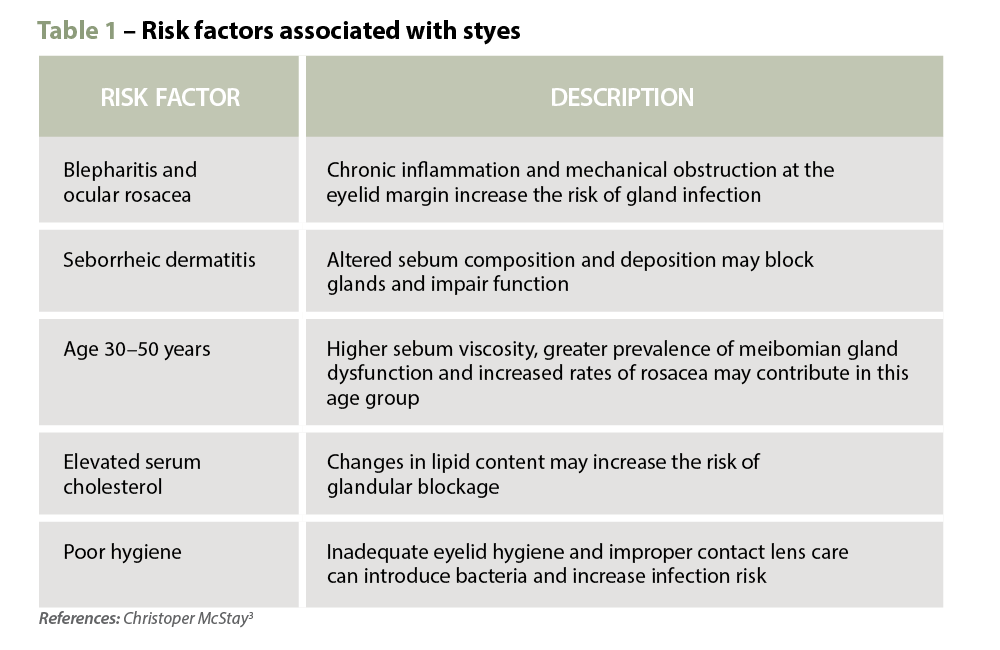
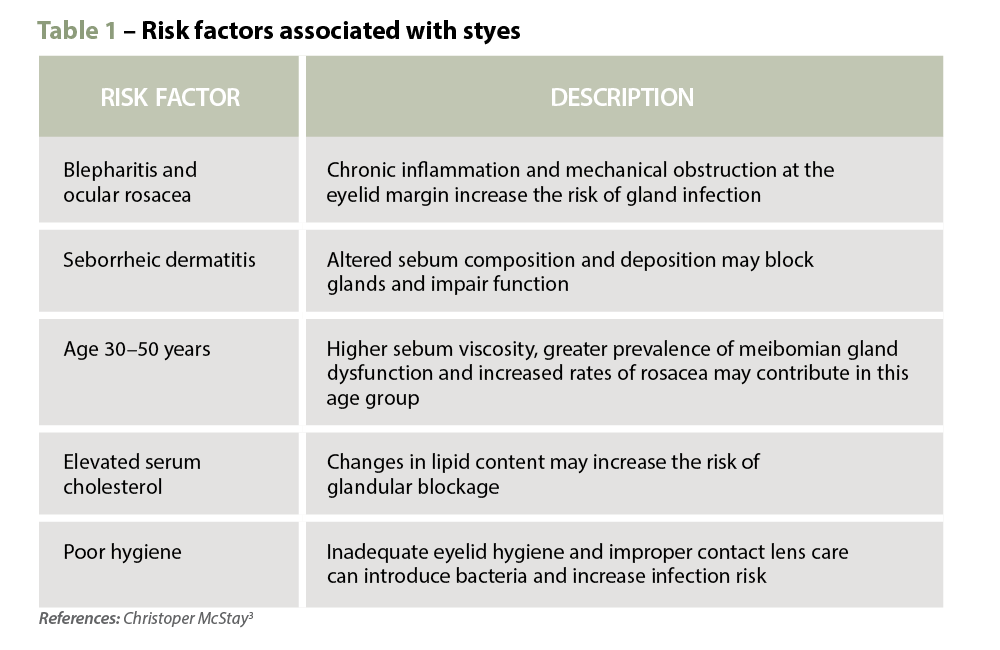
Several risk factors that are associated with the development of styes are summarised in Table 1.
 Clinical features
Clinical features A stye typically presents as a localised, tender, red and swollen mass at or near the eyelid margin, often accompanied by pain or soreness.2 While the progression of a stye may vary slightly between individuals, it generally follows the following timeline4:
When assessing eyelid lesions, it is important to distinguish a stye from a chalazion. A chalazion is a non-infectious, focal inflammatory lesion of the eyelid. It results from obstruction of the meibomian glands, with subsequent thickening and stagnation of the gland’s oily secretions, which then triggers a granulomatous inflammatory reaction.5 Unlike styes, chalazia typically form deeper within the eyelid, are often painless, and lack the characteristic pustule. If an eyelid lump does not develop a pustule and is located closer to the centre of the eyelid, it is more likely to be a chalazion. Chalazia are generally smooth and non-tender, unless complicated by secondary inflammation.6
Preseptal cellulitis is a potential complication of styes, affecting the eyelid and surrounding skin. It is typically managed with oral antibiotics in combination with warm compresses and eyelid massage.1 Preseptal cellulitis can quickly progress to orbital cellulitis, where infection extends beyond the orbital septum.1 Orbital cellulitis is a medical emergency; if left untreated, it can result in vision loss, sepsis or death.6 Key features include reduced visual acuity, severe or persistent headache and signs such as proptosis (bulging eye), painful or restrictive eye movement, ophthalmoplegia and diplopia (double vision).6 Unlike orbital cellulitis, a stye does not cause eye movement restriction or deep orbital pain.7
Immediate referral to the emergency department is warranted if orbital cellulitis is suspected or the patient appears systemically unwell (e.g. fever, lethargy). Otherwise, referral to an optometrist or a general practitioner is appropriate if1,6,7:
Most styes resolve spontaneously without pharmacological treatment. Topical or systemic antibiotics are not routinely indicated unless there are signs of secondary cellulitis involving the surrounding skin. Non-pharmacological strategies focus on relieving symptoms, promoting drainage, and preventing complications or recurrence.
 Warm compresses are the cornerstone of treatment, helping to soften the lesion, bring pus to the surface and encourage spontaneous drainage. A clean face cloth soaked in warm (not hot) water should be applied to the closed eyelid for 2–5 minutes, twice daily during the active phase. Once the stye begins to drain, any discharge should be gently wiped away using a clean, warm washcloth. After resolution, continuing warm compresses once daily may help prevent recurrence.2
Warm compresses are the cornerstone of treatment, helping to soften the lesion, bring pus to the surface and encourage spontaneous drainage. A clean face cloth soaked in warm (not hot) water should be applied to the closed eyelid for 2–5 minutes, twice daily during the active phase. Once the stye begins to drain, any discharge should be gently wiped away using a clean, warm washcloth. After resolution, continuing warm compresses once daily may help prevent recurrence.2
Maintaining good eyelid hygiene is essential both during and after treatment. Patients can clean eyelids using a damp cotton pad soaked in a diluted baby shampoo solution (e.g. 1 part shampoo to 10 parts water) or a commercial eyelid cleanser.2 Patients should be advised to avoid touching, rubbing or squeezing the stye, as this may worsen inflammation or introduce secondary infection.
Lifestyle modifications also play an important role in managing styes and preventing recurrence. Patients who wear contact lenses should be reminded to wash their hands thoroughly before handling lenses, avoid lens wear during active infection, and clean lenses and cases regularly. It is also advisable to avoid applying eye makeup on the affected eyelid, as it can introduce bacteria and cause further irritation. To reduce the risk of spreading infection, patients should use separate, clean towels and cleansing tools, avoiding sharing these items with others.
Pharmacists in primary care are well equipped to support patients presenting with a stye through early recognition, appropriate referral and evidence-based management advice. They play a key role in identifying symptoms, distinguishing between styes and more serious conditions, recommending non-pharmacological management strategies, and providing practical education on eyelid hygiene and self-care. Pharmacists should also encourage patients to consult their optometrist or general practitioner if symptoms worsen, fail to improve within a few days, or if the styes are recurrent, as this may indicate an underlying condition requiring further evaluation.
Styes are a common and generally self-limiting eyelid condition that can often be effectively managed with simple measures. Pharmacists play a vital role in assessing, educating and guiding patients in managing styes while ensuring timely referral when red flags are present. By understanding the clinical presentation, recommending appropriate treatment, and recognising when escalation is required, pharmacists contribute meaningfully to primary eye care and patient safety. Strengthening pharmacy practice with clinical insight into conditions like styes not only improves individual patient outcomes but also reinforces the pharmacist’s role as an essential part of the multidisciplinary healthcare team.
Case scenario continuedYou explore Leila’s symptoms in more detail and explain that she most likely has a stye, which is a common and usually self-limiting eyelid infection. You explain to her that topical antibiotics are not typically indicated and recommend applying warm compresses to the affected eye twice daily, maintaining good eyelid hygiene and minimising contact lens use and eye makeup until the stye resolves. You also explain the warning signs, including vision changes, painful eye movements and systemic infection symptoms, that would require immediate medical attention. Leila returns a week later to thank you, reporting that her stye has resolved completely following your advice. |
Hui Wen Quek BPharm(Hons), GradCertAppPharmPrac is a pharmacist and PhD candidate at the University of Western Australia (UWA).
Dr Amy Page PhD, MClinPharm, GradDipBiostat, GCertHProfEd, GAICD, GStat, FSHPA, FPS is a consultant pharmacist, biostatistician, and the director of the Centre for Optimisation of Medicines at UWA’s School of Allied Health.
Diyar Emadi BPharm MPS CredPharm (MMR) CDE CPT SCOPE certified MBA
Hui Wen Quek is supported by an Australian Government Research Training Program (RTP) Scholarship at the University of Western Australia.
[post_title] => Stye no more: a practical guide for management [post_excerpt] => Styes are a common and generally self-limiting eyelid condition that can often be effectively managed with simple measures. [post_status] => publish [comment_status] => open [ping_status] => open [post_password] => [post_name] => stye-no-more-a-practical-guide-for-management [to_ping] => [pinged] => [post_modified] => 2025-12-08 16:34:57 [post_modified_gmt] => 2025-12-08 05:34:57 [post_content_filtered] => [post_parent] => 0 [guid] => https://www.australianpharmacist.com.au/?p=30876 [menu_order] => 0 [post_type] => post [post_mime_type] => [comment_count] => 0 [filter] => raw ) [title_attribute] => Stye no more: a practical guide for management [title] => Stye no more: a practical guide for management [href] => https://www.australianpharmacist.com.au/stye-no-more-a-practical-guide-for-management/ [module_atts:td_module:private] => Array ( ) [td_review:protected] => Array ( [td_post_template] => single_template_4 ) [is_review:protected] => [post_thumb_id:protected] => 31030 [authorType] => )td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31089
[post_author] => 3387
[post_date] => 2025-12-15 16:54:53
[post_date_gmt] => 2025-12-15 05:54:53
[post_content] => New year, new policy and practice changes. Here’s what pharmacists will need to navigate from January.
In 2026, pharmacists can expect some changes to education, medicine costs and credentialing standards.
AP has rounded up the key changes pharmacists can expect from 1 January.
1. PBS co‑payment will drop
From 1 January 2026, the maximum Pharmaceutical Benefits Scheme (PBS) co‑payment for general patients will drop from $31.60 to $25.00 per prescription.
This marks a major reduction in out-of-pocket costs for Australians without a concession card, and the first time in more than 20 years that PBS medicines will cost no more than $25.
However, indexation on the general patient co-payment will resume in 2027 in line with the Consumer Price Index (CPI). Although PBS medicines will not be permanently capped at $25, the long‑term trajectory of general patient co‑payments will rise from a much lower baseline.
2. Transition to the new MMR credential must be completed
By 1 January 2026, pharmacists must have transitioned to the APC’s new Medication Management Review credential to continue:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31095
[post_author] => 9164
[post_date] => 2025-12-15 13:10:40
[post_date_gmt] => 2025-12-15 02:10:40
[post_content] => The Pharmaceutical Society of Australia (PSA) recently launched the PSA Standards for Continuing Professional Development (CPD) for Pharmacists, marking a new era for the accreditation of CPD activities for the pharmacy profession.
The launch of the PSA Standards follows the retirement of the Australian Pharmacy Council (APC) Accreditation Standards for CPD Activities on 31 December 2025. Developed through extensive consultation with the profession, the PSA Standards provide a contemporary framework to guide the quality and educational integrity of continuing professional development activities for pharmacists.
With the commencement of these Standards, CPD providers can apply for accreditation under the PSA Accredited CPD framework.
All supporting materials, including application forms and the PSA Accredited CPD Provider Handbook, will be available on the PSA website from 5 January 2026.
PSA acknowledges and thanks the individuals and organisations who contributed feedback during the consultation process and looks forward to supporting providers in delivering high-quality education for pharmacists.
PSA National President Associate Professor Fei Sim FPS reflected on the process of developing the Standards, acknowledging the work of all involved, including the individuals and organisations who provided feedback during the consultation period.
“The approval of the PSA standards for CPD for pharmacists marks a significant milestone in PSA’s already rich history in upholding quality education standards, now spanning decades,” she said.
“We know our education and continuing professional development are core values for our members. I want to assure you that these standards will give pharmacists the confidence that the CPD they access is of high quality.
“I sincerely thank everyone who participated in the consultation process. It is an incredible achievement to be sharing this news only 5 months after announcing PSA’s intent to publish these education standards.”
To view the Standards or enquire about the accreditation process, please visit https://www.psa.org.au/cpd/
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 30937
[post_author] => 250
[post_date] => 2025-12-10 12:05:46
[post_date_gmt] => 2025-12-10 01:05:46
[post_content] => From emergency contraception to migraines, advance supply can be appropriate. Here’s how to decide when it is – and isn’t.
It might sound like an odd request. Someone requesting a Pharmacist Only Medicine (S3) to have on hand for anticipated use in the future, rather than to respond to a current ailment or symptom. Is this allowed? And if so, when is it appropriate?
Is advance provision of S3s legal?
The answer is a (qualified) yes. While one of the primary reasons a medicine may be listed in Schedule 3 of the SUSMP,1 no Australian jurisdiction restricts advance provision of Pharmacist Only Medicines (see table).
But don’t we need to assess a patient’s therapeutic need?
Yes, the pharmacist must be satisfied there is a therapeutic need for the S3 medicine. This is mandated both in the Professional Practice Standards 2023, as well as (most) state and territory poisons regulations.
However, that therapeutic need doesn’t necessarily need to be for immediate treatment.
There will be circumstances where a therapeutic need for future use exists. For example, the APF2 treatment guidelines for emergency contraception, adrenaline and cold sores supports advance provision.
Similarly, there are cases – albeit less frequently – where advance provision is appropriate for treatment of conditions such as migraine, hives, allergic rhinitis or nasal congestion.
So when is advanced supply of S3 OK?
Quite often, but not always. Advance provision is most appropriate where a patient will need the medicine as time-sensitive treatment for a flare-up of a condition or expected recurrence of an ailment.
Advance provision is also more appropriate where a patient is unlikely to have reasonable access to a pharmacy, which is not limited to international travel.
Advance provision may not be appropriate where the patient may not be able to self-assess appropriate treatment for symptoms after counselling, where a therapeutic need does not exist, or if you believe there is a strong risk of diversion (although this is rare).
What other things do I need to consider?
There are a few, including:
These factors should be addressed in discussion with the patient when advance provision occurs.
As an opioid analogue for treatment of dry cough, it will be pretty unlikely a patient will have a reasonable therapeutic need for advance provision of dihydrocodeine syrup.
However, each request should be considered on its own merits. There will be isolated cases where it is appropriate.
| ACT3 | No comparable criteria |
| NSW4 | · pharmacist gives the person an opportunity to seek advice as to the use of the substance · quantity, or for a purpose must accord with the recognised therapeutic standard of what is appropriate in the circumstances |
| NT5 | · pharmacist must not intentionally supply to a person in a manner reckless to their circumstance |
| QLD6 | · pharmacist reasonably believes the patient has a therapeutic need |
| SA | No comparable criteria |
| TAS7 | · pharmacist forms the opinion use in the treatment of the patient is justified on consideration of the condition, disease or symptoms of the person |
| VIC8 | · for treatment of a patient under pharmacist’s care · pharmacist has taken all reasonable steps to ensure a therapeutic need exists |
| WA9 | No comparable criteria |
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31034
[post_author] => 3410
[post_date] => 2025-12-08 14:06:18
[post_date_gmt] => 2025-12-08 03:06:18
[post_content] => Professor Mark Naunton MPS, Chair of the Faculty of Health and Professor of Pharmacy at the University of Canberra, was unanimously elected by the PSA Board to serve as the next president from January 2026.
The Board has also elected Bridget Totterman MPS as National Vice President (elect) to fill the vacancy created by Prof Naunton’s election.
[caption id="attachment_31037" align="aligncenter" width="600"] Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
What motivated you to seek election as the next PSA National President?
I’ve had a long career in pharmacy, working across academia, research and education – but like most pharmacists, I started in community pharmacy.
As an intern, my preceptor was a PSA branch committee member and he paid for my PSA membership. From the very beginning, it was instilled in me how important it is to give back to the profession.
In research, I saw firsthand the gaps in our healthcare system, which drove me to explore how pharmacists can help to improve care – particularly in transitions of care. I’ve also worked in educational outreach with GPs and pharmacists, showing me how much GPs actually value pharmacists; when we communicate well and have something reasonable to say, they listen. That has always been my experience as a forward-facing clinical pharmacist
My shift into academia was driven by wanting to train the next generation of pharmacists. What I often saw in students wasn’t a lack of knowledge, but a lack of confidence – something I’m keen to address.
A consistent theme throughout my career has been the dedication of pharmacists – and how much more we could achieve with recognition, support and the right structures in place.
I’ve always wanted to use my voice to ensure our profession is heard at the highest level. I believe PSA must continue to lead with strength, vision and, above all, unity – so that our profession can not only cope with change, but thrive through it.
What do you hope to achieve as PSA President?
Recognition and remuneration that truly reflects our expertise as medicines experts are big priorities. We have a highly predominantly female workforce, including PSA’s board. There are pay inequities affecting female pharmacists that must be addressed.
I also want to strengthen PSA’s role as the national leader in pharmacy advocacy. Under Associate Professor Fei Sim’s tenure, PSA has grown significantly in this space, and I want to build on that legacy by ensuring every pharmacist feels supported, valued and confident in their practice.
That includes pharmacists across all settings – from community to hospital, general practice, aged care, academia, industry and government. We need to support and recognise the whole profession.
Fei has been a truly inspirational leader, overseeing the negotiation of the first Strategic Agreement of Pharmacist Professional Practice, establishing the PSA Foundation, driving the strategic agenda for innovation in quality use of medicines, and driving practice forward through her membership of numerous government advisory committees.
[caption id="attachment_31039" align="aligncenter" width="600"] A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
Why do you feel this is such a pivotal moment for PSA and the profession?
The PSA is undergoing a major acquisition of the Australasian College of Pharmacy. Our members voted for it because they believe it’s in the best interests of PSA and the profession, helping us strengthen advocacy, improve our education platform, expand resources, and grow our membership.
Through the acquisition, we also want education and member benefits to become more affordable for pharmacists. Cost-of-living pressures are very real, and we need members to feel that PSA genuinely has their back, making their job easier so they can practise to full scope.
At the same time, healthcare is evolving rapidly. Patients need more accessible and innovative care, with pharmacists uniquely positioned to meet those needs.
Primary care reform is happening now – and this is the moment for PSA to champion pharmacists and ensure we’re at the centre of tomorrow’s healthcare system.
What are the major challenges pharmacists are facing right now?
Workforce sustainability is, and will continue to be a significant issue now and into the near future.
While recognition of our clinical expertise is improving, especially with expanded scope of practice and pharmacist prescribing, it's still new – with awareness and acceptance being ongoing challenges.
COVID-19 highlighted what pharmacists can do exceptionally well, particularly vaccinations.
But pharmacists are stretched, with many competing demands taking a toll. Ensuring pharmacists are properly remunerated and supported is critical to maintaining the sustainability of the profession. My role is to ensure they have a voice at every level.
How do you see the profession evolving in 5 years?
Five years ago, we were doing little more than flu vaccinations. Now we’re administering a much broader range of vaccines nationally. Governments are increasingly looking for more efficient healthcare delivery, and pharmacists have shown we can answer that call. But to continue along this path, we need better-trained pharmacy assistants, because pharmacists can’t do more unless we hand over some tasks.
Another area where we still need to make headway is medicine safety. Pharmacists are trained to ensure patients get the right medicine at the right time, and we have highly skilled pharmacists providing medicines reviews – yet many are constrained by caps and limits that make no sense clinically.
In 5 years’ time, I want to see those barriers gone, so patients can actually receive the expertise pharmacists are ready and willing to provide.
I also want to see pharmacists better integrated into healthcare teams, both physically and digitally. That might mean pharmacists embedded in general practice, or pharmacists who are digitally connected to practices and other care settings. We’re a large country and we know there is a shortage of pharmacists – so we have to find creative ways to connect our expertise to where it’s needed.
How have your background and previous experiences shaped your views of the profession?
I grew up in rural Tasmania and have done a lot of work across rural and regional Australia. I know those communities don’t always feel supported. I understand the challenges facing patients, healthcare workers and pharmacists in those areas, and I want them to know that I hear them.
I’d like people in rural and regional communities to feel they can pick up the phone and talk to me – and to see me as someone who genuinely has their back, just as much as pharmacists in our cities.
I’ve also lived and worked in the Netherlands, where they have often been at the forefront of innovation in data and system design. They have shown what’s possible when you really line up systems to support better care.
I’d like to draw on those experiences and share them with the right people here, because I believe we can learn a great deal from our overseas counterparts as we strengthen pharmacy practice and medicine safety in Australia.
[post_title] => PSA’s new president wants to transform the profession
[post_excerpt] => PSA's new President, Professor Mark Naunton MPS, was unanimously elected by the Board to serve as the next president from January 2026.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => psas-new-president-wants-to-transform-the-profession
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-08 16:08:27
[post_modified_gmt] => 2025-12-08 05:08:27
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31034
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => PSA’s new president wants to transform the profession
[title] => PSA’s new president wants to transform the profession
[href] => https://www.australianpharmacist.com.au/psas-new-president-wants-to-transform-the-profession/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31035
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 30876
[post_author] => 10832
[post_date] => 2025-12-06 15:41:09
[post_date_gmt] => 2025-12-06 04:41:09
[post_content] => Case scenario
Leila, a 35-year-old woman, presents to the pharmacy concerned about a painful red bump near the margin of her upper eyelid. She explains that it appeared 2 days ago and has become increasingly tender, but she has not sought any treatment yet. Leila wears contact lenses and applies eye makeup daily. On further questioning, you learn that she is not taking any regular medications, has no underlying medical conditions, and this is the first time she has experienced such symptoms. She asks if there is anything she can apply to help.
Learning objectivesAfter reading this article, pharmacists should be able to:
|
A hordeolum, commonly known as a stye, is a common eyelid condition caused by bacterial infection of the sebaceous glands. There are two main types: external hordeolum, the more common form, which affects glands near the lash line; and internal hordeolum, which involves the meibomian glands deeper within the eyelid. Although typically benign and self-limiting, a stye is among the more common eyelid conditions seen in primary care.1 It can cause significant discomfort and cosmetic concern for patients. Most cases resolve spontaneously, but referral to a medical practitioner may be warranted in certain circumstances.
Styes are a frequent presentation in community practice, where pharmacists are well equipped to provide reassurance, advise on conservative management, reinforce good eyelid hygiene, and recognise when referral is needed. This article provides an overview of the clinical features of styes, outlines referral criteria, explores management strategies, and highlights the important role pharmacists play in supporting patients with this common condition.
An external hordeolum arises from obstruction and secondary infection of the glands of Zeis or Moll, located along the eyelid margin. In contrast, an internal hordeolum is less common and results from infection of the meibomian gland, situated deeper within the tarsal plate of the eyelid. Staphylococcus aureus is the pathogen most frequently implicated, and styes may also occur secondary to blepharitis, a chronic inflammatory condition of the eyelid.2
Several risk factors that are associated with the development of styes are summarised in Table 1.
 Clinical features
Clinical features A stye typically presents as a localised, tender, red and swollen mass at or near the eyelid margin, often accompanied by pain or soreness.2 While the progression of a stye may vary slightly between individuals, it generally follows the following timeline4:
When assessing eyelid lesions, it is important to distinguish a stye from a chalazion. A chalazion is a non-infectious, focal inflammatory lesion of the eyelid. It results from obstruction of the meibomian glands, with subsequent thickening and stagnation of the gland’s oily secretions, which then triggers a granulomatous inflammatory reaction.5 Unlike styes, chalazia typically form deeper within the eyelid, are often painless, and lack the characteristic pustule. If an eyelid lump does not develop a pustule and is located closer to the centre of the eyelid, it is more likely to be a chalazion. Chalazia are generally smooth and non-tender, unless complicated by secondary inflammation.6
Preseptal cellulitis is a potential complication of styes, affecting the eyelid and surrounding skin. It is typically managed with oral antibiotics in combination with warm compresses and eyelid massage.1 Preseptal cellulitis can quickly progress to orbital cellulitis, where infection extends beyond the orbital septum.1 Orbital cellulitis is a medical emergency; if left untreated, it can result in vision loss, sepsis or death.6 Key features include reduced visual acuity, severe or persistent headache and signs such as proptosis (bulging eye), painful or restrictive eye movement, ophthalmoplegia and diplopia (double vision).6 Unlike orbital cellulitis, a stye does not cause eye movement restriction or deep orbital pain.7
Immediate referral to the emergency department is warranted if orbital cellulitis is suspected or the patient appears systemically unwell (e.g. fever, lethargy). Otherwise, referral to an optometrist or a general practitioner is appropriate if1,6,7:
Most styes resolve spontaneously without pharmacological treatment. Topical or systemic antibiotics are not routinely indicated unless there are signs of secondary cellulitis involving the surrounding skin. Non-pharmacological strategies focus on relieving symptoms, promoting drainage, and preventing complications or recurrence.
 Warm compresses are the cornerstone of treatment, helping to soften the lesion, bring pus to the surface and encourage spontaneous drainage. A clean face cloth soaked in warm (not hot) water should be applied to the closed eyelid for 2–5 minutes, twice daily during the active phase. Once the stye begins to drain, any discharge should be gently wiped away using a clean, warm washcloth. After resolution, continuing warm compresses once daily may help prevent recurrence.2
Warm compresses are the cornerstone of treatment, helping to soften the lesion, bring pus to the surface and encourage spontaneous drainage. A clean face cloth soaked in warm (not hot) water should be applied to the closed eyelid for 2–5 minutes, twice daily during the active phase. Once the stye begins to drain, any discharge should be gently wiped away using a clean, warm washcloth. After resolution, continuing warm compresses once daily may help prevent recurrence.2
Maintaining good eyelid hygiene is essential both during and after treatment. Patients can clean eyelids using a damp cotton pad soaked in a diluted baby shampoo solution (e.g. 1 part shampoo to 10 parts water) or a commercial eyelid cleanser.2 Patients should be advised to avoid touching, rubbing or squeezing the stye, as this may worsen inflammation or introduce secondary infection.
Lifestyle modifications also play an important role in managing styes and preventing recurrence. Patients who wear contact lenses should be reminded to wash their hands thoroughly before handling lenses, avoid lens wear during active infection, and clean lenses and cases regularly. It is also advisable to avoid applying eye makeup on the affected eyelid, as it can introduce bacteria and cause further irritation. To reduce the risk of spreading infection, patients should use separate, clean towels and cleansing tools, avoiding sharing these items with others.
Pharmacists in primary care are well equipped to support patients presenting with a stye through early recognition, appropriate referral and evidence-based management advice. They play a key role in identifying symptoms, distinguishing between styes and more serious conditions, recommending non-pharmacological management strategies, and providing practical education on eyelid hygiene and self-care. Pharmacists should also encourage patients to consult their optometrist or general practitioner if symptoms worsen, fail to improve within a few days, or if the styes are recurrent, as this may indicate an underlying condition requiring further evaluation.
Styes are a common and generally self-limiting eyelid condition that can often be effectively managed with simple measures. Pharmacists play a vital role in assessing, educating and guiding patients in managing styes while ensuring timely referral when red flags are present. By understanding the clinical presentation, recommending appropriate treatment, and recognising when escalation is required, pharmacists contribute meaningfully to primary eye care and patient safety. Strengthening pharmacy practice with clinical insight into conditions like styes not only improves individual patient outcomes but also reinforces the pharmacist’s role as an essential part of the multidisciplinary healthcare team.
Case scenario continuedYou explore Leila’s symptoms in more detail and explain that she most likely has a stye, which is a common and usually self-limiting eyelid infection. You explain to her that topical antibiotics are not typically indicated and recommend applying warm compresses to the affected eye twice daily, maintaining good eyelid hygiene and minimising contact lens use and eye makeup until the stye resolves. You also explain the warning signs, including vision changes, painful eye movements and systemic infection symptoms, that would require immediate medical attention. Leila returns a week later to thank you, reporting that her stye has resolved completely following your advice. |
Hui Wen Quek BPharm(Hons), GradCertAppPharmPrac is a pharmacist and PhD candidate at the University of Western Australia (UWA).
Dr Amy Page PhD, MClinPharm, GradDipBiostat, GCertHProfEd, GAICD, GStat, FSHPA, FPS is a consultant pharmacist, biostatistician, and the director of the Centre for Optimisation of Medicines at UWA’s School of Allied Health.
Diyar Emadi BPharm MPS CredPharm (MMR) CDE CPT SCOPE certified MBA
Hui Wen Quek is supported by an Australian Government Research Training Program (RTP) Scholarship at the University of Western Australia.
[post_title] => Stye no more: a practical guide for management [post_excerpt] => Styes are a common and generally self-limiting eyelid condition that can often be effectively managed with simple measures. [post_status] => publish [comment_status] => open [ping_status] => open [post_password] => [post_name] => stye-no-more-a-practical-guide-for-management [to_ping] => [pinged] => [post_modified] => 2025-12-08 16:34:57 [post_modified_gmt] => 2025-12-08 05:34:57 [post_content_filtered] => [post_parent] => 0 [guid] => https://www.australianpharmacist.com.au/?p=30876 [menu_order] => 0 [post_type] => post [post_mime_type] => [comment_count] => 0 [filter] => raw ) [title_attribute] => Stye no more: a practical guide for management [title] => Stye no more: a practical guide for management [href] => https://www.australianpharmacist.com.au/stye-no-more-a-practical-guide-for-management/ [module_atts:td_module:private] => Array ( ) [td_review:protected] => Array ( [td_post_template] => single_template_4 ) [is_review:protected] => [post_thumb_id:protected] => 31030 [authorType] => )td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31089
[post_author] => 3387
[post_date] => 2025-12-15 16:54:53
[post_date_gmt] => 2025-12-15 05:54:53
[post_content] => New year, new policy and practice changes. Here’s what pharmacists will need to navigate from January.
In 2026, pharmacists can expect some changes to education, medicine costs and credentialing standards.
AP has rounded up the key changes pharmacists can expect from 1 January.
1. PBS co‑payment will drop
From 1 January 2026, the maximum Pharmaceutical Benefits Scheme (PBS) co‑payment for general patients will drop from $31.60 to $25.00 per prescription.
This marks a major reduction in out-of-pocket costs for Australians without a concession card, and the first time in more than 20 years that PBS medicines will cost no more than $25.
However, indexation on the general patient co-payment will resume in 2027 in line with the Consumer Price Index (CPI). Although PBS medicines will not be permanently capped at $25, the long‑term trajectory of general patient co‑payments will rise from a much lower baseline.
2. Transition to the new MMR credential must be completed
By 1 January 2026, pharmacists must have transitioned to the APC’s new Medication Management Review credential to continue:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31095
[post_author] => 9164
[post_date] => 2025-12-15 13:10:40
[post_date_gmt] => 2025-12-15 02:10:40
[post_content] => The Pharmaceutical Society of Australia (PSA) recently launched the PSA Standards for Continuing Professional Development (CPD) for Pharmacists, marking a new era for the accreditation of CPD activities for the pharmacy profession.
The launch of the PSA Standards follows the retirement of the Australian Pharmacy Council (APC) Accreditation Standards for CPD Activities on 31 December 2025. Developed through extensive consultation with the profession, the PSA Standards provide a contemporary framework to guide the quality and educational integrity of continuing professional development activities for pharmacists.
With the commencement of these Standards, CPD providers can apply for accreditation under the PSA Accredited CPD framework.
All supporting materials, including application forms and the PSA Accredited CPD Provider Handbook, will be available on the PSA website from 5 January 2026.
PSA acknowledges and thanks the individuals and organisations who contributed feedback during the consultation process and looks forward to supporting providers in delivering high-quality education for pharmacists.
PSA National President Associate Professor Fei Sim FPS reflected on the process of developing the Standards, acknowledging the work of all involved, including the individuals and organisations who provided feedback during the consultation period.
“The approval of the PSA standards for CPD for pharmacists marks a significant milestone in PSA’s already rich history in upholding quality education standards, now spanning decades,” she said.
“We know our education and continuing professional development are core values for our members. I want to assure you that these standards will give pharmacists the confidence that the CPD they access is of high quality.
“I sincerely thank everyone who participated in the consultation process. It is an incredible achievement to be sharing this news only 5 months after announcing PSA’s intent to publish these education standards.”
To view the Standards or enquire about the accreditation process, please visit https://www.psa.org.au/cpd/
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 30937
[post_author] => 250
[post_date] => 2025-12-10 12:05:46
[post_date_gmt] => 2025-12-10 01:05:46
[post_content] => From emergency contraception to migraines, advance supply can be appropriate. Here’s how to decide when it is – and isn’t.
It might sound like an odd request. Someone requesting a Pharmacist Only Medicine (S3) to have on hand for anticipated use in the future, rather than to respond to a current ailment or symptom. Is this allowed? And if so, when is it appropriate?
Is advance provision of S3s legal?
The answer is a (qualified) yes. While one of the primary reasons a medicine may be listed in Schedule 3 of the SUSMP,1 no Australian jurisdiction restricts advance provision of Pharmacist Only Medicines (see table).
But don’t we need to assess a patient’s therapeutic need?
Yes, the pharmacist must be satisfied there is a therapeutic need for the S3 medicine. This is mandated both in the Professional Practice Standards 2023, as well as (most) state and territory poisons regulations.
However, that therapeutic need doesn’t necessarily need to be for immediate treatment.
There will be circumstances where a therapeutic need for future use exists. For example, the APF2 treatment guidelines for emergency contraception, adrenaline and cold sores supports advance provision.
Similarly, there are cases – albeit less frequently – where advance provision is appropriate for treatment of conditions such as migraine, hives, allergic rhinitis or nasal congestion.
So when is advanced supply of S3 OK?
Quite often, but not always. Advance provision is most appropriate where a patient will need the medicine as time-sensitive treatment for a flare-up of a condition or expected recurrence of an ailment.
Advance provision is also more appropriate where a patient is unlikely to have reasonable access to a pharmacy, which is not limited to international travel.
Advance provision may not be appropriate where the patient may not be able to self-assess appropriate treatment for symptoms after counselling, where a therapeutic need does not exist, or if you believe there is a strong risk of diversion (although this is rare).
What other things do I need to consider?
There are a few, including:
These factors should be addressed in discussion with the patient when advance provision occurs.
As an opioid analogue for treatment of dry cough, it will be pretty unlikely a patient will have a reasonable therapeutic need for advance provision of dihydrocodeine syrup.
However, each request should be considered on its own merits. There will be isolated cases where it is appropriate.
| ACT3 | No comparable criteria |
| NSW4 | · pharmacist gives the person an opportunity to seek advice as to the use of the substance · quantity, or for a purpose must accord with the recognised therapeutic standard of what is appropriate in the circumstances |
| NT5 | · pharmacist must not intentionally supply to a person in a manner reckless to their circumstance |
| QLD6 | · pharmacist reasonably believes the patient has a therapeutic need |
| SA | No comparable criteria |
| TAS7 | · pharmacist forms the opinion use in the treatment of the patient is justified on consideration of the condition, disease or symptoms of the person |
| VIC8 | · for treatment of a patient under pharmacist’s care · pharmacist has taken all reasonable steps to ensure a therapeutic need exists |
| WA9 | No comparable criteria |
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31034
[post_author] => 3410
[post_date] => 2025-12-08 14:06:18
[post_date_gmt] => 2025-12-08 03:06:18
[post_content] => Professor Mark Naunton MPS, Chair of the Faculty of Health and Professor of Pharmacy at the University of Canberra, was unanimously elected by the PSA Board to serve as the next president from January 2026.
The Board has also elected Bridget Totterman MPS as National Vice President (elect) to fill the vacancy created by Prof Naunton’s election.
[caption id="attachment_31037" align="aligncenter" width="600"] Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
What motivated you to seek election as the next PSA National President?
I’ve had a long career in pharmacy, working across academia, research and education – but like most pharmacists, I started in community pharmacy.
As an intern, my preceptor was a PSA branch committee member and he paid for my PSA membership. From the very beginning, it was instilled in me how important it is to give back to the profession.
In research, I saw firsthand the gaps in our healthcare system, which drove me to explore how pharmacists can help to improve care – particularly in transitions of care. I’ve also worked in educational outreach with GPs and pharmacists, showing me how much GPs actually value pharmacists; when we communicate well and have something reasonable to say, they listen. That has always been my experience as a forward-facing clinical pharmacist
My shift into academia was driven by wanting to train the next generation of pharmacists. What I often saw in students wasn’t a lack of knowledge, but a lack of confidence – something I’m keen to address.
A consistent theme throughout my career has been the dedication of pharmacists – and how much more we could achieve with recognition, support and the right structures in place.
I’ve always wanted to use my voice to ensure our profession is heard at the highest level. I believe PSA must continue to lead with strength, vision and, above all, unity – so that our profession can not only cope with change, but thrive through it.
What do you hope to achieve as PSA President?
Recognition and remuneration that truly reflects our expertise as medicines experts are big priorities. We have a highly predominantly female workforce, including PSA’s board. There are pay inequities affecting female pharmacists that must be addressed.
I also want to strengthen PSA’s role as the national leader in pharmacy advocacy. Under Associate Professor Fei Sim’s tenure, PSA has grown significantly in this space, and I want to build on that legacy by ensuring every pharmacist feels supported, valued and confident in their practice.
That includes pharmacists across all settings – from community to hospital, general practice, aged care, academia, industry and government. We need to support and recognise the whole profession.
Fei has been a truly inspirational leader, overseeing the negotiation of the first Strategic Agreement of Pharmacist Professional Practice, establishing the PSA Foundation, driving the strategic agenda for innovation in quality use of medicines, and driving practice forward through her membership of numerous government advisory committees.
[caption id="attachment_31039" align="aligncenter" width="600"] A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
Why do you feel this is such a pivotal moment for PSA and the profession?
The PSA is undergoing a major acquisition of the Australasian College of Pharmacy. Our members voted for it because they believe it’s in the best interests of PSA and the profession, helping us strengthen advocacy, improve our education platform, expand resources, and grow our membership.
Through the acquisition, we also want education and member benefits to become more affordable for pharmacists. Cost-of-living pressures are very real, and we need members to feel that PSA genuinely has their back, making their job easier so they can practise to full scope.
At the same time, healthcare is evolving rapidly. Patients need more accessible and innovative care, with pharmacists uniquely positioned to meet those needs.
Primary care reform is happening now – and this is the moment for PSA to champion pharmacists and ensure we’re at the centre of tomorrow’s healthcare system.
What are the major challenges pharmacists are facing right now?
Workforce sustainability is, and will continue to be a significant issue now and into the near future.
While recognition of our clinical expertise is improving, especially with expanded scope of practice and pharmacist prescribing, it's still new – with awareness and acceptance being ongoing challenges.
COVID-19 highlighted what pharmacists can do exceptionally well, particularly vaccinations.
But pharmacists are stretched, with many competing demands taking a toll. Ensuring pharmacists are properly remunerated and supported is critical to maintaining the sustainability of the profession. My role is to ensure they have a voice at every level.
How do you see the profession evolving in 5 years?
Five years ago, we were doing little more than flu vaccinations. Now we’re administering a much broader range of vaccines nationally. Governments are increasingly looking for more efficient healthcare delivery, and pharmacists have shown we can answer that call. But to continue along this path, we need better-trained pharmacy assistants, because pharmacists can’t do more unless we hand over some tasks.
Another area where we still need to make headway is medicine safety. Pharmacists are trained to ensure patients get the right medicine at the right time, and we have highly skilled pharmacists providing medicines reviews – yet many are constrained by caps and limits that make no sense clinically.
In 5 years’ time, I want to see those barriers gone, so patients can actually receive the expertise pharmacists are ready and willing to provide.
I also want to see pharmacists better integrated into healthcare teams, both physically and digitally. That might mean pharmacists embedded in general practice, or pharmacists who are digitally connected to practices and other care settings. We’re a large country and we know there is a shortage of pharmacists – so we have to find creative ways to connect our expertise to where it’s needed.
How have your background and previous experiences shaped your views of the profession?
I grew up in rural Tasmania and have done a lot of work across rural and regional Australia. I know those communities don’t always feel supported. I understand the challenges facing patients, healthcare workers and pharmacists in those areas, and I want them to know that I hear them.
I’d like people in rural and regional communities to feel they can pick up the phone and talk to me – and to see me as someone who genuinely has their back, just as much as pharmacists in our cities.
I’ve also lived and worked in the Netherlands, where they have often been at the forefront of innovation in data and system design. They have shown what’s possible when you really line up systems to support better care.
I’d like to draw on those experiences and share them with the right people here, because I believe we can learn a great deal from our overseas counterparts as we strengthen pharmacy practice and medicine safety in Australia.
[post_title] => PSA’s new president wants to transform the profession
[post_excerpt] => PSA's new President, Professor Mark Naunton MPS, was unanimously elected by the Board to serve as the next president from January 2026.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => psas-new-president-wants-to-transform-the-profession
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-08 16:08:27
[post_modified_gmt] => 2025-12-08 05:08:27
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31034
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => PSA’s new president wants to transform the profession
[title] => PSA’s new president wants to transform the profession
[href] => https://www.australianpharmacist.com.au/psas-new-president-wants-to-transform-the-profession/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31035
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 30876
[post_author] => 10832
[post_date] => 2025-12-06 15:41:09
[post_date_gmt] => 2025-12-06 04:41:09
[post_content] => Case scenario
Leila, a 35-year-old woman, presents to the pharmacy concerned about a painful red bump near the margin of her upper eyelid. She explains that it appeared 2 days ago and has become increasingly tender, but she has not sought any treatment yet. Leila wears contact lenses and applies eye makeup daily. On further questioning, you learn that she is not taking any regular medications, has no underlying medical conditions, and this is the first time she has experienced such symptoms. She asks if there is anything she can apply to help.
Learning objectivesAfter reading this article, pharmacists should be able to:
|
A hordeolum, commonly known as a stye, is a common eyelid condition caused by bacterial infection of the sebaceous glands. There are two main types: external hordeolum, the more common form, which affects glands near the lash line; and internal hordeolum, which involves the meibomian glands deeper within the eyelid. Although typically benign and self-limiting, a stye is among the more common eyelid conditions seen in primary care.1 It can cause significant discomfort and cosmetic concern for patients. Most cases resolve spontaneously, but referral to a medical practitioner may be warranted in certain circumstances.
Styes are a frequent presentation in community practice, where pharmacists are well equipped to provide reassurance, advise on conservative management, reinforce good eyelid hygiene, and recognise when referral is needed. This article provides an overview of the clinical features of styes, outlines referral criteria, explores management strategies, and highlights the important role pharmacists play in supporting patients with this common condition.
An external hordeolum arises from obstruction and secondary infection of the glands of Zeis or Moll, located along the eyelid margin. In contrast, an internal hordeolum is less common and results from infection of the meibomian gland, situated deeper within the tarsal plate of the eyelid. Staphylococcus aureus is the pathogen most frequently implicated, and styes may also occur secondary to blepharitis, a chronic inflammatory condition of the eyelid.2
Several risk factors that are associated with the development of styes are summarised in Table 1.
 Clinical features
Clinical features A stye typically presents as a localised, tender, red and swollen mass at or near the eyelid margin, often accompanied by pain or soreness.2 While the progression of a stye may vary slightly between individuals, it generally follows the following timeline4:
When assessing eyelid lesions, it is important to distinguish a stye from a chalazion. A chalazion is a non-infectious, focal inflammatory lesion of the eyelid. It results from obstruction of the meibomian glands, with subsequent thickening and stagnation of the gland’s oily secretions, which then triggers a granulomatous inflammatory reaction.5 Unlike styes, chalazia typically form deeper within the eyelid, are often painless, and lack the characteristic pustule. If an eyelid lump does not develop a pustule and is located closer to the centre of the eyelid, it is more likely to be a chalazion. Chalazia are generally smooth and non-tender, unless complicated by secondary inflammation.6
Preseptal cellulitis is a potential complication of styes, affecting the eyelid and surrounding skin. It is typically managed with oral antibiotics in combination with warm compresses and eyelid massage.1 Preseptal cellulitis can quickly progress to orbital cellulitis, where infection extends beyond the orbital septum.1 Orbital cellulitis is a medical emergency; if left untreated, it can result in vision loss, sepsis or death.6 Key features include reduced visual acuity, severe or persistent headache and signs such as proptosis (bulging eye), painful or restrictive eye movement, ophthalmoplegia and diplopia (double vision).6 Unlike orbital cellulitis, a stye does not cause eye movement restriction or deep orbital pain.7
Immediate referral to the emergency department is warranted if orbital cellulitis is suspected or the patient appears systemically unwell (e.g. fever, lethargy). Otherwise, referral to an optometrist or a general practitioner is appropriate if1,6,7:
Most styes resolve spontaneously without pharmacological treatment. Topical or systemic antibiotics are not routinely indicated unless there are signs of secondary cellulitis involving the surrounding skin. Non-pharmacological strategies focus on relieving symptoms, promoting drainage, and preventing complications or recurrence.
 Warm compresses are the cornerstone of treatment, helping to soften the lesion, bring pus to the surface and encourage spontaneous drainage. A clean face cloth soaked in warm (not hot) water should be applied to the closed eyelid for 2–5 minutes, twice daily during the active phase. Once the stye begins to drain, any discharge should be gently wiped away using a clean, warm washcloth. After resolution, continuing warm compresses once daily may help prevent recurrence.2
Warm compresses are the cornerstone of treatment, helping to soften the lesion, bring pus to the surface and encourage spontaneous drainage. A clean face cloth soaked in warm (not hot) water should be applied to the closed eyelid for 2–5 minutes, twice daily during the active phase. Once the stye begins to drain, any discharge should be gently wiped away using a clean, warm washcloth. After resolution, continuing warm compresses once daily may help prevent recurrence.2
Maintaining good eyelid hygiene is essential both during and after treatment. Patients can clean eyelids using a damp cotton pad soaked in a diluted baby shampoo solution (e.g. 1 part shampoo to 10 parts water) or a commercial eyelid cleanser.2 Patients should be advised to avoid touching, rubbing or squeezing the stye, as this may worsen inflammation or introduce secondary infection.
Lifestyle modifications also play an important role in managing styes and preventing recurrence. Patients who wear contact lenses should be reminded to wash their hands thoroughly before handling lenses, avoid lens wear during active infection, and clean lenses and cases regularly. It is also advisable to avoid applying eye makeup on the affected eyelid, as it can introduce bacteria and cause further irritation. To reduce the risk of spreading infection, patients should use separate, clean towels and cleansing tools, avoiding sharing these items with others.
Pharmacists in primary care are well equipped to support patients presenting with a stye through early recognition, appropriate referral and evidence-based management advice. They play a key role in identifying symptoms, distinguishing between styes and more serious conditions, recommending non-pharmacological management strategies, and providing practical education on eyelid hygiene and self-care. Pharmacists should also encourage patients to consult their optometrist or general practitioner if symptoms worsen, fail to improve within a few days, or if the styes are recurrent, as this may indicate an underlying condition requiring further evaluation.
Styes are a common and generally self-limiting eyelid condition that can often be effectively managed with simple measures. Pharmacists play a vital role in assessing, educating and guiding patients in managing styes while ensuring timely referral when red flags are present. By understanding the clinical presentation, recommending appropriate treatment, and recognising when escalation is required, pharmacists contribute meaningfully to primary eye care and patient safety. Strengthening pharmacy practice with clinical insight into conditions like styes not only improves individual patient outcomes but also reinforces the pharmacist’s role as an essential part of the multidisciplinary healthcare team.
Case scenario continuedYou explore Leila’s symptoms in more detail and explain that she most likely has a stye, which is a common and usually self-limiting eyelid infection. You explain to her that topical antibiotics are not typically indicated and recommend applying warm compresses to the affected eye twice daily, maintaining good eyelid hygiene and minimising contact lens use and eye makeup until the stye resolves. You also explain the warning signs, including vision changes, painful eye movements and systemic infection symptoms, that would require immediate medical attention. Leila returns a week later to thank you, reporting that her stye has resolved completely following your advice. |
Hui Wen Quek BPharm(Hons), GradCertAppPharmPrac is a pharmacist and PhD candidate at the University of Western Australia (UWA).
Dr Amy Page PhD, MClinPharm, GradDipBiostat, GCertHProfEd, GAICD, GStat, FSHPA, FPS is a consultant pharmacist, biostatistician, and the director of the Centre for Optimisation of Medicines at UWA’s School of Allied Health.
Diyar Emadi BPharm MPS CredPharm (MMR) CDE CPT SCOPE certified MBA
Hui Wen Quek is supported by an Australian Government Research Training Program (RTP) Scholarship at the University of Western Australia.
[post_title] => Stye no more: a practical guide for management [post_excerpt] => Styes are a common and generally self-limiting eyelid condition that can often be effectively managed with simple measures. [post_status] => publish [comment_status] => open [ping_status] => open [post_password] => [post_name] => stye-no-more-a-practical-guide-for-management [to_ping] => [pinged] => [post_modified] => 2025-12-08 16:34:57 [post_modified_gmt] => 2025-12-08 05:34:57 [post_content_filtered] => [post_parent] => 0 [guid] => https://www.australianpharmacist.com.au/?p=30876 [menu_order] => 0 [post_type] => post [post_mime_type] => [comment_count] => 0 [filter] => raw ) [title_attribute] => Stye no more: a practical guide for management [title] => Stye no more: a practical guide for management [href] => https://www.australianpharmacist.com.au/stye-no-more-a-practical-guide-for-management/ [module_atts:td_module:private] => Array ( ) [td_review:protected] => Array ( [td_post_template] => single_template_4 ) [is_review:protected] => [post_thumb_id:protected] => 31030 [authorType] => )td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31089
[post_author] => 3387
[post_date] => 2025-12-15 16:54:53
[post_date_gmt] => 2025-12-15 05:54:53
[post_content] => New year, new policy and practice changes. Here’s what pharmacists will need to navigate from January.
In 2026, pharmacists can expect some changes to education, medicine costs and credentialing standards.
AP has rounded up the key changes pharmacists can expect from 1 January.
1. PBS co‑payment will drop
From 1 January 2026, the maximum Pharmaceutical Benefits Scheme (PBS) co‑payment for general patients will drop from $31.60 to $25.00 per prescription.
This marks a major reduction in out-of-pocket costs for Australians without a concession card, and the first time in more than 20 years that PBS medicines will cost no more than $25.
However, indexation on the general patient co-payment will resume in 2027 in line with the Consumer Price Index (CPI). Although PBS medicines will not be permanently capped at $25, the long‑term trajectory of general patient co‑payments will rise from a much lower baseline.
2. Transition to the new MMR credential must be completed
By 1 January 2026, pharmacists must have transitioned to the APC’s new Medication Management Review credential to continue:
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31095
[post_author] => 9164
[post_date] => 2025-12-15 13:10:40
[post_date_gmt] => 2025-12-15 02:10:40
[post_content] => The Pharmaceutical Society of Australia (PSA) recently launched the PSA Standards for Continuing Professional Development (CPD) for Pharmacists, marking a new era for the accreditation of CPD activities for the pharmacy profession.
The launch of the PSA Standards follows the retirement of the Australian Pharmacy Council (APC) Accreditation Standards for CPD Activities on 31 December 2025. Developed through extensive consultation with the profession, the PSA Standards provide a contemporary framework to guide the quality and educational integrity of continuing professional development activities for pharmacists.
With the commencement of these Standards, CPD providers can apply for accreditation under the PSA Accredited CPD framework.
All supporting materials, including application forms and the PSA Accredited CPD Provider Handbook, will be available on the PSA website from 5 January 2026.
PSA acknowledges and thanks the individuals and organisations who contributed feedback during the consultation process and looks forward to supporting providers in delivering high-quality education for pharmacists.
PSA National President Associate Professor Fei Sim FPS reflected on the process of developing the Standards, acknowledging the work of all involved, including the individuals and organisations who provided feedback during the consultation period.
“The approval of the PSA standards for CPD for pharmacists marks a significant milestone in PSA’s already rich history in upholding quality education standards, now spanning decades,” she said.
“We know our education and continuing professional development are core values for our members. I want to assure you that these standards will give pharmacists the confidence that the CPD they access is of high quality.
“I sincerely thank everyone who participated in the consultation process. It is an incredible achievement to be sharing this news only 5 months after announcing PSA’s intent to publish these education standards.”
To view the Standards or enquire about the accreditation process, please visit https://www.psa.org.au/cpd/
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 30937
[post_author] => 250
[post_date] => 2025-12-10 12:05:46
[post_date_gmt] => 2025-12-10 01:05:46
[post_content] => From emergency contraception to migraines, advance supply can be appropriate. Here’s how to decide when it is – and isn’t.
It might sound like an odd request. Someone requesting a Pharmacist Only Medicine (S3) to have on hand for anticipated use in the future, rather than to respond to a current ailment or symptom. Is this allowed? And if so, when is it appropriate?
Is advance provision of S3s legal?
The answer is a (qualified) yes. While one of the primary reasons a medicine may be listed in Schedule 3 of the SUSMP,1 no Australian jurisdiction restricts advance provision of Pharmacist Only Medicines (see table).
But don’t we need to assess a patient’s therapeutic need?
Yes, the pharmacist must be satisfied there is a therapeutic need for the S3 medicine. This is mandated both in the Professional Practice Standards 2023, as well as (most) state and territory poisons regulations.
However, that therapeutic need doesn’t necessarily need to be for immediate treatment.
There will be circumstances where a therapeutic need for future use exists. For example, the APF2 treatment guidelines for emergency contraception, adrenaline and cold sores supports advance provision.
Similarly, there are cases – albeit less frequently – where advance provision is appropriate for treatment of conditions such as migraine, hives, allergic rhinitis or nasal congestion.
So when is advanced supply of S3 OK?
Quite often, but not always. Advance provision is most appropriate where a patient will need the medicine as time-sensitive treatment for a flare-up of a condition or expected recurrence of an ailment.
Advance provision is also more appropriate where a patient is unlikely to have reasonable access to a pharmacy, which is not limited to international travel.
Advance provision may not be appropriate where the patient may not be able to self-assess appropriate treatment for symptoms after counselling, where a therapeutic need does not exist, or if you believe there is a strong risk of diversion (although this is rare).
What other things do I need to consider?
There are a few, including:
These factors should be addressed in discussion with the patient when advance provision occurs.
As an opioid analogue for treatment of dry cough, it will be pretty unlikely a patient will have a reasonable therapeutic need for advance provision of dihydrocodeine syrup.
However, each request should be considered on its own merits. There will be isolated cases where it is appropriate.
| ACT3 | No comparable criteria |
| NSW4 | · pharmacist gives the person an opportunity to seek advice as to the use of the substance · quantity, or for a purpose must accord with the recognised therapeutic standard of what is appropriate in the circumstances |
| NT5 | · pharmacist must not intentionally supply to a person in a manner reckless to their circumstance |
| QLD6 | · pharmacist reasonably believes the patient has a therapeutic need |
| SA | No comparable criteria |
| TAS7 | · pharmacist forms the opinion use in the treatment of the patient is justified on consideration of the condition, disease or symptoms of the person |
| VIC8 | · for treatment of a patient under pharmacist’s care · pharmacist has taken all reasonable steps to ensure a therapeutic need exists |
| WA9 | No comparable criteria |
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 31034
[post_author] => 3410
[post_date] => 2025-12-08 14:06:18
[post_date_gmt] => 2025-12-08 03:06:18
[post_content] => Professor Mark Naunton MPS, Chair of the Faculty of Health and Professor of Pharmacy at the University of Canberra, was unanimously elected by the PSA Board to serve as the next president from January 2026.
The Board has also elected Bridget Totterman MPS as National Vice President (elect) to fill the vacancy created by Prof Naunton’s election.
[caption id="attachment_31037" align="aligncenter" width="600"] Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
Team PSA 2026: Caroline Diamantis FPS, Prof Mark Naunton MPS and Bridget Totterman MPS[/caption]
AP sat down with the incoming national president for an exclusive interview on how he plans to lead and support the profession.
What motivated you to seek election as the next PSA National President?
I’ve had a long career in pharmacy, working across academia, research and education – but like most pharmacists, I started in community pharmacy.
As an intern, my preceptor was a PSA branch committee member and he paid for my PSA membership. From the very beginning, it was instilled in me how important it is to give back to the profession.
In research, I saw firsthand the gaps in our healthcare system, which drove me to explore how pharmacists can help to improve care – particularly in transitions of care. I’ve also worked in educational outreach with GPs and pharmacists, showing me how much GPs actually value pharmacists; when we communicate well and have something reasonable to say, they listen. That has always been my experience as a forward-facing clinical pharmacist
My shift into academia was driven by wanting to train the next generation of pharmacists. What I often saw in students wasn’t a lack of knowledge, but a lack of confidence – something I’m keen to address.
A consistent theme throughout my career has been the dedication of pharmacists – and how much more we could achieve with recognition, support and the right structures in place.
I’ve always wanted to use my voice to ensure our profession is heard at the highest level. I believe PSA must continue to lead with strength, vision and, above all, unity – so that our profession can not only cope with change, but thrive through it.
What do you hope to achieve as PSA President?
Recognition and remuneration that truly reflects our expertise as medicines experts are big priorities. We have a highly predominantly female workforce, including PSA’s board. There are pay inequities affecting female pharmacists that must be addressed.
I also want to strengthen PSA’s role as the national leader in pharmacy advocacy. Under Associate Professor Fei Sim’s tenure, PSA has grown significantly in this space, and I want to build on that legacy by ensuring every pharmacist feels supported, valued and confident in their practice.
That includes pharmacists across all settings – from community to hospital, general practice, aged care, academia, industry and government. We need to support and recognise the whole profession.
Fei has been a truly inspirational leader, overseeing the negotiation of the first Strategic Agreement of Pharmacist Professional Practice, establishing the PSA Foundation, driving the strategic agenda for innovation in quality use of medicines, and driving practice forward through her membership of numerous government advisory committees.
[caption id="attachment_31039" align="aligncenter" width="600"] A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
A/Prof Fei Sim and Prof Mark Naunton[/caption]
Most of all, she is loved by the profession, and is held in the highest esteem by pharmacists from all areas of practice, the PSA Board and by external stakeholders.
Why do you feel this is such a pivotal moment for PSA and the profession?
The PSA is undergoing a major acquisition of the Australasian College of Pharmacy. Our members voted for it because they believe it’s in the best interests of PSA and the profession, helping us strengthen advocacy, improve our education platform, expand resources, and grow our membership.
Through the acquisition, we also want education and member benefits to become more affordable for pharmacists. Cost-of-living pressures are very real, and we need members to feel that PSA genuinely has their back, making their job easier so they can practise to full scope.
At the same time, healthcare is evolving rapidly. Patients need more accessible and innovative care, with pharmacists uniquely positioned to meet those needs.
Primary care reform is happening now – and this is the moment for PSA to champion pharmacists and ensure we’re at the centre of tomorrow’s healthcare system.
What are the major challenges pharmacists are facing right now?
Workforce sustainability is, and will continue to be a significant issue now and into the near future.
While recognition of our clinical expertise is improving, especially with expanded scope of practice and pharmacist prescribing, it's still new – with awareness and acceptance being ongoing challenges.
COVID-19 highlighted what pharmacists can do exceptionally well, particularly vaccinations.
But pharmacists are stretched, with many competing demands taking a toll. Ensuring pharmacists are properly remunerated and supported is critical to maintaining the sustainability of the profession. My role is to ensure they have a voice at every level.
How do you see the profession evolving in 5 years?
Five years ago, we were doing little more than flu vaccinations. Now we’re administering a much broader range of vaccines nationally. Governments are increasingly looking for more efficient healthcare delivery, and pharmacists have shown we can answer that call. But to continue along this path, we need better-trained pharmacy assistants, because pharmacists can’t do more unless we hand over some tasks.
Another area where we still need to make headway is medicine safety. Pharmacists are trained to ensure patients get the right medicine at the right time, and we have highly skilled pharmacists providing medicines reviews – yet many are constrained by caps and limits that make no sense clinically.
In 5 years’ time, I want to see those barriers gone, so patients can actually receive the expertise pharmacists are ready and willing to provide.
I also want to see pharmacists better integrated into healthcare teams, both physically and digitally. That might mean pharmacists embedded in general practice, or pharmacists who are digitally connected to practices and other care settings. We’re a large country and we know there is a shortage of pharmacists – so we have to find creative ways to connect our expertise to where it’s needed.
How have your background and previous experiences shaped your views of the profession?
I grew up in rural Tasmania and have done a lot of work across rural and regional Australia. I know those communities don’t always feel supported. I understand the challenges facing patients, healthcare workers and pharmacists in those areas, and I want them to know that I hear them.
I’d like people in rural and regional communities to feel they can pick up the phone and talk to me – and to see me as someone who genuinely has their back, just as much as pharmacists in our cities.
I’ve also lived and worked in the Netherlands, where they have often been at the forefront of innovation in data and system design. They have shown what’s possible when you really line up systems to support better care.
I’d like to draw on those experiences and share them with the right people here, because I believe we can learn a great deal from our overseas counterparts as we strengthen pharmacy practice and medicine safety in Australia.
[post_title] => PSA’s new president wants to transform the profession
[post_excerpt] => PSA's new President, Professor Mark Naunton MPS, was unanimously elected by the Board to serve as the next president from January 2026.
[post_status] => publish
[comment_status] => open
[ping_status] => open
[post_password] =>
[post_name] => psas-new-president-wants-to-transform-the-profession
[to_ping] =>
[pinged] =>
[post_modified] => 2025-12-08 16:08:27
[post_modified_gmt] => 2025-12-08 05:08:27
[post_content_filtered] =>
[post_parent] => 0
[guid] => https://www.australianpharmacist.com.au/?p=31034
[menu_order] => 0
[post_type] => post
[post_mime_type] =>
[comment_count] => 0
[filter] => raw
)
[title_attribute] => PSA’s new president wants to transform the profession
[title] => PSA’s new president wants to transform the profession
[href] => https://www.australianpharmacist.com.au/psas-new-president-wants-to-transform-the-profession/
[module_atts:td_module:private] => Array
(
)
[td_review:protected] => Array
(
)
[is_review:protected] =>
[post_thumb_id:protected] => 31035
[authorType] =>
)
td_module_mega_menu Object
(
[post] => WP_Post Object
(
[ID] => 30876
[post_author] => 10832
[post_date] => 2025-12-06 15:41:09
[post_date_gmt] => 2025-12-06 04:41:09
[post_content] => Case scenario
Leila, a 35-year-old woman, presents to the pharmacy concerned about a painful red bump near the margin of her upper eyelid. She explains that it appeared 2 days ago and has become increasingly tender, but she has not sought any treatment yet. Leila wears contact lenses and applies eye makeup daily. On further questioning, you learn that she is not taking any regular medications, has no underlying medical conditions, and this is the first time she has experienced such symptoms. She asks if there is anything she can apply to help.
Learning objectivesAfter reading this article, pharmacists should be able to:
|
A hordeolum, commonly known as a stye, is a common eyelid condition caused by bacterial infection of the sebaceous glands. There are two main types: external hordeolum, the more common form, which affects glands near the lash line; and internal hordeolum, which involves the meibomian glands deeper within the eyelid. Although typically benign and self-limiting, a stye is among the more common eyelid conditions seen in primary care.1 It can cause significant discomfort and cosmetic concern for patients. Most cases resolve spontaneously, but referral to a medical practitioner may be warranted in certain circumstances.
Styes are a frequent presentation in community practice, where pharmacists are well equipped to provide reassurance, advise on conservative management, reinforce good eyelid hygiene, and recognise when referral is needed. This article provides an overview of the clinical features of styes, outlines referral criteria, explores management strategies, and highlights the important role pharmacists play in supporting patients with this common condition.
An external hordeolum arises from obstruction and secondary infection of the glands of Zeis or Moll, located along the eyelid margin. In contrast, an internal hordeolum is less common and results from infection of the meibomian gland, situated deeper within the tarsal plate of the eyelid. Staphylococcus aureus is the pathogen most frequently implicated, and styes may also occur secondary to blepharitis, a chronic inflammatory condition of the eyelid.2
Several risk factors that are associated with the development of styes are summarised in Table 1.
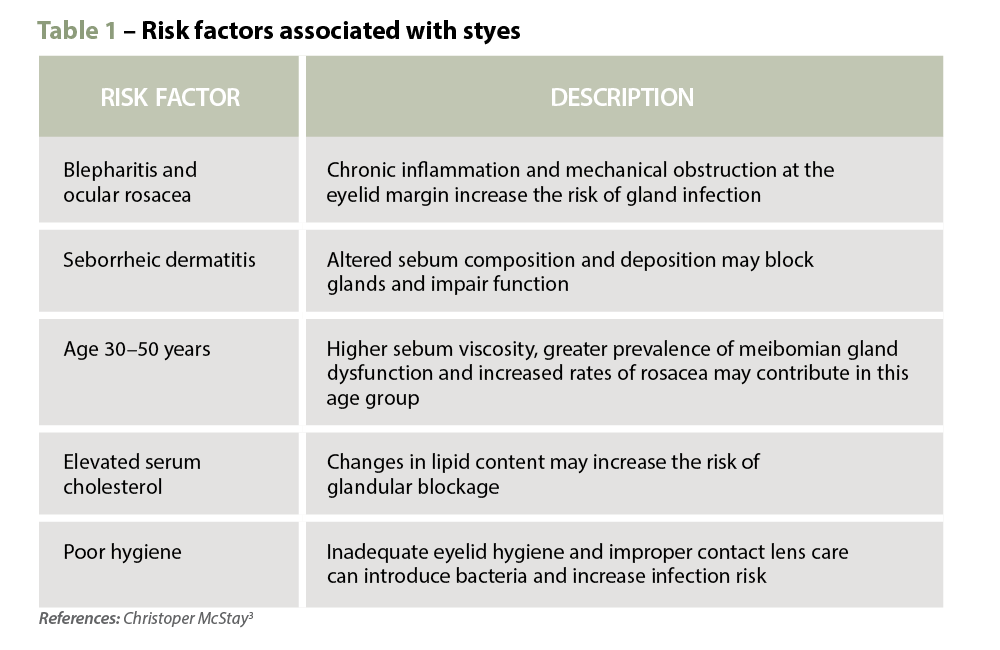 Clinical features
Clinical features A stye typically presents as a localised, tender, red and swollen mass at or near the eyelid margin, often accompanied by pain or soreness.2 While the progression of a stye may vary slightly between individuals, it generally follows the following timeline4:
When assessing eyelid lesions, it is important to distinguish a stye from a chalazion. A chalazion is a non-infectious, focal inflammatory lesion of the eyelid. It results from obstruction of the meibomian glands, with subsequent thickening and stagnation of the gland’s oily secretions, which then triggers a granulomatous inflammatory reaction.5 Unlike styes, chalazia typically form deeper within the eyelid, are often painless, and lack the characteristic pustule. If an eyelid lump does not develop a pustule and is located closer to the centre of the eyelid, it is more likely to be a chalazion. Chalazia are generally smooth and non-tender, unless complicated by secondary inflammation.6
Preseptal cellulitis is a potential complication of styes, affecting the eyelid and surrounding skin. It is typically managed with oral antibiotics in combination with warm compresses and eyelid massage.1 Preseptal cellulitis can quickly progress to orbital cellulitis, where infection extends beyond the orbital septum.1 Orbital cellulitis is a medical emergency; if left untreated, it can result in vision loss, sepsis or death.6 Key features include reduced visual acuity, severe or persistent headache and signs such as proptosis (bulging eye), painful or restrictive eye movement, ophthalmoplegia and diplopia (double vision).6 Unlike orbital cellulitis, a stye does not cause eye movement restriction or deep orbital pain.7
Immediate referral to the emergency department is warranted if orbital cellulitis is suspected or the patient appears systemically unwell (e.g. fever, lethargy). Otherwise, referral to an optometrist or a general practitioner is appropriate if1,6,7:
Most styes resolve spontaneously without pharmacological treatment. Topical or systemic antibiotics are not routinely indicated unless there are signs of secondary cellulitis involving the surrounding skin. Non-pharmacological strategies focus on relieving symptoms, promoting drainage, and preventing complications or recurrence.
 Warm compresses are the cornerstone of treatment, helping to soften the lesion, bring pus to the surface and encourage spontaneous drainage. A clean face cloth soaked in warm (not hot) water should be applied to the closed eyelid for 2–5 minutes, twice daily during the active phase. Once the stye begins to drain, any discharge should be gently wiped away using a clean, warm washcloth. After resolution, continuing warm compresses once daily may help prevent recurrence.2
Warm compresses are the cornerstone of treatment, helping to soften the lesion, bring pus to the surface and encourage spontaneous drainage. A clean face cloth soaked in warm (not hot) water should be applied to the closed eyelid for 2–5 minutes, twice daily during the active phase. Once the stye begins to drain, any discharge should be gently wiped away using a clean, warm washcloth. After resolution, continuing warm compresses once daily may help prevent recurrence.2
Maintaining good eyelid hygiene is essential both during and after treatment. Patients can clean eyelids using a damp cotton pad soaked in a diluted baby shampoo solution (e.g. 1 part shampoo to 10 parts water) or a commercial eyelid cleanser.2 Patients should be advised to avoid touching, rubbing or squeezing the stye, as this may worsen inflammation or introduce secondary infection.
Lifestyle modifications also play an important role in managing styes and preventing recurrence. Patients who wear contact lenses should be reminded to wash their hands thoroughly before handling lenses, avoid lens wear during active infection, and clean lenses and cases regularly. It is also advisable to avoid applying eye makeup on the affected eyelid, as it can introduce bacteria and cause further irritation. To reduce the risk of spreading infection, patients should use separate, clean towels and cleansing tools, avoiding sharing these items with others.
Pharmacists in primary care are well equipped to support patients presenting with a stye through early recognition, appropriate referral and evidence-based management advice. They play a key role in identifying symptoms, distinguishing between styes and more serious conditions, recommending non-pharmacological management strategies, and providing practical education on eyelid hygiene and self-care. Pharmacists should also encourage patients to consult their optometrist or general practitioner if symptoms worsen, fail to improve within a few days, or if the styes are recurrent, as this may indicate an underlying condition requiring further evaluation.
Styes are a common and generally self-limiting eyelid condition that can often be effectively managed with simple measures. Pharmacists play a vital role in assessing, educating and guiding patients in managing styes while ensuring timely referral when red flags are present. By understanding the clinical presentation, recommending appropriate treatment, and recognising when escalation is required, pharmacists contribute meaningfully to primary eye care and patient safety. Strengthening pharmacy practice with clinical insight into conditions like styes not only improves individual patient outcomes but also reinforces the pharmacist’s role as an essential part of the multidisciplinary healthcare team.
Case scenario continuedYou explore Leila’s symptoms in more detail and explain that she most likely has a stye, which is a common and usually self-limiting eyelid infection. You explain to her that topical antibiotics are not typically indicated and recommend applying warm compresses to the affected eye twice daily, maintaining good eyelid hygiene and minimising contact lens use and eye makeup until the stye resolves. You also explain the warning signs, including vision changes, painful eye movements and systemic infection symptoms, that would require immediate medical attention. Leila returns a week later to thank you, reporting that her stye has resolved completely following your advice. |
Hui Wen Quek BPharm(Hons), GradCertAppPharmPrac is a pharmacist and PhD candidate at the University of Western Australia (UWA).
Dr Amy Page PhD, MClinPharm, GradDipBiostat, GCertHProfEd, GAICD, GStat, FSHPA, FPS is a consultant pharmacist, biostatistician, and the director of the Centre for Optimisation of Medicines at UWA’s School of Allied Health.
Diyar Emadi BPharm MPS CredPharm (MMR) CDE CPT SCOPE certified MBA
Hui Wen Quek is supported by an Australian Government Research Training Program (RTP) Scholarship at the University of Western Australia.
[post_title] => Stye no more: a practical guide for management [post_excerpt] => Styes are a common and generally self-limiting eyelid condition that can often be effectively managed with simple measures. [post_status] => publish [comment_status] => open [ping_status] => open [post_password] => [post_name] => stye-no-more-a-practical-guide-for-management [to_ping] => [pinged] => [post_modified] => 2025-12-08 16:34:57 [post_modified_gmt] => 2025-12-08 05:34:57 [post_content_filtered] => [post_parent] => 0 [guid] => https://www.australianpharmacist.com.au/?p=30876 [menu_order] => 0 [post_type] => post [post_mime_type] => [comment_count] => 0 [filter] => raw ) [title_attribute] => Stye no more: a practical guide for management [title] => Stye no more: a practical guide for management [href] => https://www.australianpharmacist.com.au/stye-no-more-a-practical-guide-for-management/ [module_atts:td_module:private] => Array ( ) [td_review:protected] => Array ( [td_post_template] => single_template_4 ) [is_review:protected] => [post_thumb_id:protected] => 31030 [authorType] => )Get your weekly dose of the news and research you need to help advance your practice.
Protected by Google reCAPTCHA v3.

Australian Pharmacist is the official journal for Pharmaceutical Society of Australia Ltd.